Aleve
Kathleen Finnegan, MS, MT(ASCP)SHCM - Clinical Associate Professor
- Chair, Clinical Laboratory Sciences Program
- State University of New York at Stony Brook
- Stony Brook, New York
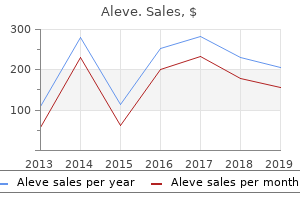
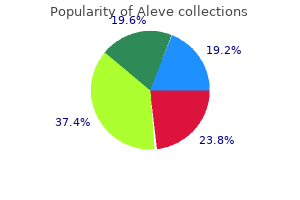
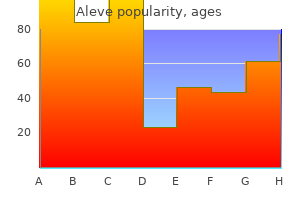
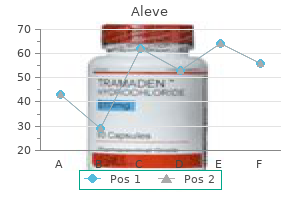
Aleve 500 mg saleAlternatively treatment of neuropathic pain guidelines purchase aleve 250mg on line, stapling of the anterior and posterior partitions can be achieved by utilizing thoracoabdominal stapler (without a cutter) introduced via enterotomy on both side best pain medication for uti order 500 mg aleve visa. Previous sclerotherapy induces periesophageal fibrosis pain treatment arthritis buy 500mg aleve with mastercard, which poses a menace of injuring the esophageal wall throughout devascularization pain treatment center fayetteville nc 500mg aleve overnight delivery. When the esophagus is infected due to a number of classes of sclerotherapy, especially in the acute setting, the stapling is done just below the gastroesophageal junction (Chaudhary & Aranya, 1991). Occasionally, fundic resection is required for bleeding from massive fundic varices (Han et al, 2004; Lee et al, 2009). Sometimes, early gastrotomy to oversew gastric varices is needed in acutely bleeding gastric varices. When the Sengstaken-Blakemore tube is used for short-term control of bleeding, we first perform the esophagogastric devascularization and splenic artery ligation without deflating the tube and later proceed to splenectomy. Placement of a feeding jejunostomy in patients with esophageal transection or stapling permits early establishment of enteral nutrition postoperatively. A gastrograffin swallow is done across the seventh postoperative day, after which oral alimentation is resumed. Kitano and colleagues (1994) first described laparoscopic assisted devascularization in seven patients with cirrhosis with bleeding esophageal varices. Manzano-Trovamala and colleagues in 1996 carried out the totally laparoscopic devascularization. Several authors have subsequently carried out a devascularization procedure by a minimal invasive strategy with a quantity of modifications, with superb results (Akahoshi et al, 2014; Cheng et al, 2014; Danis et al, 2004; Helmy et al, 2003; Wang et al, 2008, 2015; Yamamoto et al, 2006; Zhao et al, 2013). Devascularization through a single port has additionally been described (Jing et al, 2013; Wu et al, 2013; Xu et al, 2014). Jiang and colleagues (2009) in contrast open and laparoscopic splenectomy with azygoportal devascularization and concluded that the laparoscopic procedure was a safe and efficient methodology in carefully chosen patients. Laparoscopic Devascularization: Procedure the affected person lies supine strapped to the desk to allow for changes in place. The patient is placed within the reverse Trendelenberg position, and the splenic hilum is uncovered by dividing the splenogastric, gastrocolic, and splenocolic ligaments. The remaining attachments (splenophrenic and splenorenal) are divided in order that the spleen now has solely the hilar attachments left. The posterior gastric vein, the primary branch of gastric coronary vein, and the left gastric artery are recognized and divided. The esophagus is pulled inferiorly, and the lower 6 to 10 cm of the esophagus is devascularized. The spleen is positioned in a retrieval bag, morcellated, and extracted from the 12 mm trocar. The head of the round stapler has been closed, and the esophageal anastomosishasbeencompleted. In a meta-analysis of those knowledge, the hemodynamic parameters confirmed a big lower of portal vein stress, portal vein diameter, and free portal strain in the combined group in contrast with the devascularization group. The authors claim that combined procedures combine the advantages of shunt surgical procedure with those of devascularization, together with sustaining the normal anatomic construction of the portal vein (Yin et al, 2013). However, we feel that it defeats the very cause of performing a devascularization procedure as an alternative of shunting, as a outcome of devascularization is usually performed in patients in whom a shunt is both not feasible or thought of to be unsafe. At finest, it might suggest that patients chosen for a shunt procedure might profit by addition of restricted devascularization. A more radical strategy, in form of partial or whole esophagogastrectomy with jejunal or colonic conduit for bypass, has been instructed by some authors (Habif, 1950; Lynn, 1971; Orloff et al, 1994; Schafer et al, 1950). These are helpful solely as the final resort in patients with extrahepatic portal obstruction with unshuntable veins and a failed devascularization procedure. The overall operative mortality fee of the Hassab procedure in Egypt (Hassab, 1967) was reported as 12. When the devascularization operation is used as an emergency procedure, the operative mortality increases significantly to 38. In sufferers with cirrhosis, the Child-Pugh status�based mortality was zero % for 244 Child-Pugh class A patients, 2% for 251 class B patients, and 16% for 176 class C sufferers. In the Western collection, the operative mortality of the operation carried out as an emergency process for variceal bleeding varied between 22% and 100% (Selzner et al, 2001). Better leads to Japanese series have been attributed to the truth that most patients with cirrhosis in Japanese collection had been nonalcoholic. Although alcohol-related continual liver disease has been thought of by some authors to be at larger danger for postoperative issues due to other coexisting ailments and malnutrition, others found no significant distinction within the outcomes of sufferers with alcoholic versus nonalcoholic cirrhosis (Rikkers et al, 1998; Selzner et al, 2001; Sugiura & Futagawa, 1973). In sufferers with cirrhosis, the main reason for mortality is hepatic decompensation and never variceal bleeding. However, in sufferers with a noncirrhotic etiology, variceal bleeding quite than liver failure is the frequent explanation for demise following acute variceal bleeding. In an evaluation of 3588 operated patients from fifty nine Japanese centers, Inokuchi (1985) reported that postoperative variceal bleeding accounted for only eight. Qazi and colleagues (2006) reported mortality in Child-Pugh A, B, and C as 12% to 14%, 30% to 50%, and 80%, respectively, for the modified Sugiura process. Operative Morbidity the outcomes, together with morbidity and mortality, in varied devascularization operations are summarized in Tables eighty four. The morbidity is said to the underlying liver dysfunction and the surgical technique used. The fee of esophageal leakage and stenosis with the Sugiura and modified Sugiura procedures incorporating esophageal transection are 5% to 14% and 2% to 28%, respectively. Some authors have suggested that avoiding esophageal transection can keep away from these issues whereas sustaining comparable rebleed rates (Johnson et al, 2006; Zhang et al, 2014). We routinely perform esophageal transection and keep away from this only in circumstances of a friable esophagus or one which has undergone latest a quantity of classes of sclerotherapy. The incidence of postoperative ascites has ranged broadly, from 3% to 33%, based on the severity of cirrhosis, extent of splanchnic venous thrombosis, and preoperative presence of ascites. In sequence reporting a excessive price of postoperative ascites, it normally resolves inside a quantity of months (Selzner et al, 2001). Portal vein thrombosis may be linked to thrombocythemia or to a decrease in portal blood move after splenectomy (Han et al 2014; Takenaka et al, 1990; Zhang et al, 2012; Zheng et al, 2013) and impacts 5. The actual fee could additionally be higher because reported charges usually include solely symptomatic cases. Unexplained fever and abdominal pain by the end of the primary postoperative week must be assessed by ultrasound Doppler and distinction computed tomography. Acute portal vein thrombosis should be treated with anticoagulation for a interval of 3 to 6 months with careful monitoring. Efficacy: Control of Variceal Hemorrhage Devascularization procedures are effective in controlling variceal bleeding. They additionally handle the underlying hypersplenism as splenectomy is a component of the process.
Buy 500mg aleve free shippingThe intrinsic veins embrace the submucosal pain treatment lexington ky buy aleve 500mg free shipping, subepithelial heel pain treatment urdu aleve 500mg low price, and the intraepithelial veins and are strongly implicated in the growth of varices treatment for pain due to uti cheap aleve 250mg on line. In portal hypertension pain medication for dogs with bite wounds discount aleve 500 mg mastercard, the elevated venous strain can produce varices throughout the length of the esophagus and down into the upper stomach; nevertheless, the bleeding from esophageal varices normally occurs in the lowest 5 cm of the esophagus. Therefore a technique focusing on this weak area would assist in controlling or preventing bleeding from esophageal varices. An perfect approach would be the everlasting obliteration or interruption of varices in the decrease periesophageal vessels and intraepithelial dilated vessels. Devascularization being a variceal-directed ablative surgery aims at obliteration of varices or disconnection of the esophagogastric veins from the hypertensive portal tributaries. The goal of the esophagogastric devascularization is to disconnect the esophagus and stomach from this collateral system while maintaining a portosystemic shunt in place through the adventitial plexus surrounding the esophagus (Spence, 1984). Most of the described devascularization procedures have two main elements, first, devascularization of the esophagogastric area to reduce bleeding from the esophagogastric varices, and second, splenectomy, which decreases portal move and thereby strain, facilitates esophagogastric devascularization, and also effectively deals with hypersplenism, if present. In the early 50s and 60s, surgery was directed toward ligation/transection of varices and esophageal transection. Boerema and Crile, in 1950, reported ligation of esophageal varices with unsatisfactory outcomes. Along related traces, gastroesophageal resection (Habif, 1950; Koop & Roddy, 1958; Lynn, 1971; Nachlas, 1956; Perry et al, 1963; Phemister & Humphrey, 1947; Schafer & Kittle, 1950), higher gastric transection (Mikkelsen & Pattisen, 1959; Schmitt & Heinrich, 1963; Tanner, 1950) and transabdominal esophageal transection (Boerema et al, 1949; Burns & Schenk, 1971) had been additionally reported in the interval, with unsatisfactory outcomes. Hepatic Cirrhosis, Portal Hypertension, and Hepatic Failure Chapter eighty four Portal hypertensive bleeding: operative devascularization 1209 In the late 60s and early 70s, Hassab and Sugiura developed the 2 successful procedures named after them that describe systematic devascularization of the esophagogastric region together with splenectomy. Hassab, in 1967, described an esophagogastric devascularization utterly performed through the belly route in portal hypertension, secondary to schistosomiasis. In 1973, Japanese surgeons Sugiura and Futagawa described a transthoracic esophageal devascularization mixed with esophageal transection and an abdominal approach for splenectomy and upper stomach devascularization with vagotomy and pyloroplasty. Hassab, 1967; and Sugiura and Futagawa, 1973; reported good outcomes and laid the foundation for the currently practiced devascularization procedures. The idea of the Sugiura procedure seemed to be extra universally accepted of the 2 approaches. Subsequently, the Sugiura procedure was modified to a single-stage abdominal process, which is the basis of the presently performed devascularization procedure and has resulted in outcomes similar to the unique transthoracic twostage process (Ginsberg et al, 1982; Hidalgo Huerta et al, 1983; Inokuchi, 1985; Jin & Rikkers, 1996; Umeyama et al, 1983; Yamamoto et al, 1976). During the final decade, devascularization procedures have also been carried out by several facilities utilizing a minimally invasive approach. Even although on this sequence the process of gastroesophageal devascularization with splenectomy was applied in cases of portal hypertension secondary to bilharzial (schistosomiasis) etiology, the procedure is really helpful for other etiologies as nicely. The choices for incision embrace midline, prolonged left subcostal, or L formed, depending on the scale of spleen. Splenectomy and ligation of short gastric veins is followed by ligation of the vessels ascending by way of the hiatus and the diaphragm. A major part of the gastrohepatic ligament containing the left gastric vessel is split between ligatures. The peritoneum over the intraabdominal a half of esophagus is reflected, and the abdominal esophagus is circumferentially dissected and looped with umbilical tape. An essential side of the Hassab procedure is the absence of esophageal transection and pyloroplasty. Hassab advised that portoazygous disconnection was adequate and esophageal transection was unnecessary. Several authors have practiced the Hassab process or modified Hassab process with good outcomes. It included 174 sufferers operated throughout or after a bleed, with 39 patients operated under emergency conditions on the time of bleeding, and in 151 patients, devascularization was carried out prophylactically. Hassab reported glorious outcomes, with an in-hospital mortality of 9% for elective instances, whereas in sufferers operated throughout bleeding in an emergency setting, the mortality was 38. Although early deadly rebleeding occurred in 8 patients, there was just one late rebleeding occasion during follow-up. The authors reported that varices disappeared fully or improved in 91% of sufferers. The process consists of a transthoracic and an abdominal procedure performed via two separate incisions. The thoracic procedure involves extensive paraesophageal devascularization as a lot as the inferior pulmonary vein and esophageal transection. The stomach procedure includes splenectomy, devascularization of the belly esophagus and cardia, and selective vagotomy and pyloroplasty. The hiatus now could be devascularized, and the lower esophagus is transected at the stage of the diaphragm. The posterior muscular layer was left intact within the unique description, and roughly 70 to ninety interrupted sutures are applied to occlude the divided varices. Sugiura-Futagawa Operation: Abdominal Procedure Laparotomy is carried out via an higher midline incision with left lateral extension. The first step is to carry out a splenectomy, adopted by devascularization of the abdominal a part of the esophagus and cardia, adopted by the higher curvature. Lesser curvature devascularization follows, and the cardioesophageal branches of left gastric vessels (but not the main left gastric) are ligated and divided. The size of devascularization is approximately 7 cm of the lesser curvature (two-thirds of lesser curvature); the lower extent of the devascularization reaches approximately the midpoint of the lesser curvature, preserving solely two descending branches of the left gastric artery. The esophagus and cardia are completely mobilized and freed from the adjoining constructions. Devascularization is facilitated by division of anterior vagus nerve, and because of this, a pyloroplasty is carried out. Thus, conceptually, the Sugiura process combines splenectomy with esophagogastric devascularization, which destroys (ligates and divides) the intraesophageal portocaval shunt but preserves periesophageal portacaval shunt, as only the perforating veins draining the esophagogastric varices are divided, and the periesophageal plexus of veins that connect the coronary venous system are preserved. The splenectomy does lower the total portal blood circulate and thereby strain, but to not the extent of a total shunt process and therefore lessens the danger of hepatic decompensation. Sugiura and Futagawa (1973) reported the disappearance of varices in 71 of seventy three survivors (97%). In the bigger expertise reported by Sugiura and Futagawa in 1984, of the 671 patients who underwent the procedure, 203 (30%) had prophylactic, 363 (54%) had elective, and a hundred and five (16%) had an emergency process. In sufferers with cirrhosis, ChildPugh status�based mortality was 0% for 244 Child-Pugh class A sufferers, 2% for 251 class B sufferers, and 16% for 176 class C sufferers. The general survival price was 46% for group C in contrast with 86% and 81% for group A and B, respectively. Late deaths were as a end result of hepatic failure and hepatocellular carcinoma and not because of variceal bleeding. The 10 year actuarial survival rate in sufferers with cirrhosis was 55% in emergency cases, 72% in prophylactic instances, and 72% in Sugiura-Futagawa Operation: Thoracic Procedure In the thoracic part of the operation, a left lateral thoracotomy is performed within the sixth intercostal area, and the mediastinal pleura is incised. Care is taken to preserve the dilated collateral veins running parallel to the esophagus, and solely the shunts (vascular channels) from these to the esophagus are utterly ligated and divided.
Order 500 mg aleve with visaTo allow for either general anesthesia or conscious sedation advanced pain institute treatment center generic aleve 500 mg on line, patients take nothing by mouth for six hours earlier than the process pain treatment for ms cheap aleve 250 mg without a prescription. They are properly hydrated and have functional venous entry marianjoy integrative pain treatment center buy aleve 500mg on-line, notably if cholangitis is a half of the medical picture treatment for long term shingles pain generic 250mg aleve fast delivery. These sufferers can turn out to be septic and hypotensive, requiring fast quantity expansion. The ability to scan the liver in a single breath hold after which cine by way of the images facilitates identification of the extent of obstruction and the chance of isolation (see Chapter 18). It additionally allows the formulation of a 3D psychological picture of the biliary tree, and understanding the biliary anatomy on this method facilitates a successful, uncomplicated procedure. It is incessantly potential to anticipate regular variants of bile duct anatomy, which might have a significant impression on preprocedure planning (see Chapter 2). Drainage Catheter Versus Primary Stent Placement the suitability of a affected person for main stent placement is decided on the time of biliary drainage based on the indication for the drainage, evidence of contaminated bile, presence of blood or tumor inside the biliary tree, and cholangiographic findings. In patients with a presumed sterile biliary tree, an try must be made to accomplish this with out ever placing a drainage catheter into the duodenum. Blood clot inside the intrahepatic bile ducts impairs drainage and might cause stent obstruction that may result in bile leaking into the peritoneal cavity from the site of duct puncture. When clots are seen throughout the biliary tree (see Chapter 125), a drainage catheter is positioned till the bile clears, at which era the patient is stented. Catheter manipulation in this group of sufferers is saved to a minimum to diminish the danger of procedure-related sepsis. Predictions concerning the degree of obstruction and degree of isolation of the biliary tree could be made primarily based on the preprocedure imaging studies. Patients with Bismuth sort I obstruction can have the whole liver drained with one catheter or stent, as a end result of proper and left ducts talk freely. Barring one of the previously mentioned contraindications, these sufferers have a main stent placed. Some recommend that survival is healthier when each side of the liver are drained (Chang et al, 1998). In either case, we choose to stent into the widespread bile duct and never into the duodenum if possible in order to protect operate of the sphincter of Oddi. One advantage of the extra anatomic Y-shaped configuration stent placement is that if stent occlusion occurs, both stents are approachable endoscopically. In this case, and in the absence of some other contraindication, a patient being drained for pruritus alone may need a main stent placed, because solely a small portion of the liver needs to be drained to alleviate pruritus. We use this as a rule of thumb, regardless of that in a collection of 149 sufferers drained at Memorial Sloan Kettering Cancer Center, we discovered solely a slightly vital distinction within the variety of patients attaining a bilirubin lower than 2 mg/dL, based mostly on the estimated quantity of liver drained. In this evaluation, 6 (29%) of 21 sufferers with less than one third of the liver drained attained a bilirubin stage below 2 mg/dL, whereas this was achieved in 65 (51%) of 128 patients with a couple of third of the liver drained (P =. After stent placement, if the bilirubin fails to fall to the desired degree, a second drainage process can be carried out. If an internal/external drainage catheter is placed, and subsequently the serum bilirubin normalizes with out evidence of cholangitis, the patient can undergo stenting of that portion of the liver drained by the catheter. When the initial drainage is on the best aspect, and the tumor has extended up the best hepatic duct in order to isolate the anterior and posterior divisions from one another and from the left hepatic duct, side-by-side self-expanding metallic stents may be positioned on the best to drain both the anterior and posterior ducts. Alternatively, when the left facet of the liver is functional, a left drainage could be performed as the following step; then one stent could be placed from the left, and one other can be positioned from the right. Although a big distinction in patency is reported when more than one stent is positioned in a noncoaxial method (Maybody et al, 2009), the mean patency of multiple stents is almost 6 months, justifying stent placement. The ideas of biliary drainage are easy, but when high bile duct obstruction is present, the planning is advanced, and execution may be troublesome. The patient will have to have sufficient of the liver drained to be free of cholangitis and pruritus and to impact a discount in serum bilirubin to receive chemotherapy, if indicated. Given that no distinction in stent patency is reported if the stent is inserted for proximal or distal obstruction, that a significant difference in patency is seen when multiple stent is placed, and that lower complication rates are reported when stents are positioned primarily, major stent placement must be considered every time possible (Inal et al, 2003a, 2003c; Maybody et al, 2009). With correct approach, together with peripheral bile duct puncture, severe bleeding complications are uncommon. Because the hepatic artery, portal vein, and bile duct journey aspect by aspect inside portal triads, blood may enter the bile duct during catheter exchanges, resulting in hemobilia within the instant postprocedure period (see Chapter 125). Hemobilia usually clears inside 24 hours, and new or recurrent hemobilia inside the first few days of drainage typically is said to catheter malposition. If the catheter is pulled out from its unique place, a catheter sidehole could become positioned adjacent to a portal vein department; this problem could be corrected by simply repositioning the catheter, but the catheter is usually upsized as nicely. No matter where the initial puncture is performed to opacify the biliary tree, makes an attempt are always made to puncture a peripheral bile duct for catheter placement, ideally a fourth-order or fifth-order department. The extra peripheral the bile duct punctured, the smaller the accompanying hepatic artery branch, and the decrease the danger of arterial damage and postprocedure bleeding. Despite prophylactic antibiotic protection, sepsis could happen instantly after or inside a number of hours of drainage and must be handled appropriately (Smith et al, 2004). This is most incessantly manifested by the development of rigors with normal or low physique temperature, however hypotension and fever may happen. Sepsis is managed with continued administration of applicable antibiotics, enlargement of intravascular volume, and pressor assist if necessary. Blood cultures must be drawn to establish organisms answerable for the bacteremia. This is particularly necessary for these with preprocedure fever, biliary-enteric anastomosis or sphincterotomy, earlier endoscopic retrograde cholangiopancreatography, or an indwelling stent or catheter. Although positive bile cultures are more frequent in sufferers with benign bile duct obstruction, cultures are optimistic in more than half of sufferers with malignant obstruction. Five p.c of patients without fever, previous biliary surgery, or endoscopic or percutaneous intervention have positive bile cultures (Brody et al, 1998). Leaking is most frequently related to the catheter turning into malpositioned in order that a number of sideholes are no longer inside the biliary tree however are within the catheter tract or even exterior the affected person. Leakage may also be seen with lack of sufficient sideholes above the level of obstruction. Anything that impedes the circulate of bile from above the obstruction, both through the catheter to below the obstruction or right into a drainage bag, will lead to bile leaking back alongside an established tract. For a correctly positioned catheter with an appropriate number of sideholes, the issue is easily remedied by catheter exchange. Patients with capped internal-external catheters might have bile leak again alongside the catheter tract when egress of bile is obstructed internally. Distal sidehole occlusion is the most typical cause, and this problem is easily remedied by catheter change. Patients with duodenal obstruction or impaired small bowel motility may be relegated to obligate exterior drainage. The best treatment is to set up internal biliary drainage with stent placement as expeditiously as possible.
Cheap 250 mg aleve amexFor patients discovered to have unresectable illness at laparotomy ocean view pain treatment center purchase 500 mg aleve with amex, cholecystectomy and operative biliary bypass with a biliary-enteric anastomosis for drainage could also be an possibility (see Chapters 31 and 42) ayurvedic back pain treatment kerala buy aleve 500mg overnight delivery. Operative biliary bypass has increased patency charges in contrast with endoscopic stenting but has increased morbidity compared with nonoperative palliation pain management for dogs with bone cancer purchase aleve 250mg amex. The complication of biliary-enteric anastomotic leak is seen 6% to 21% of patients innovative pain treatment surgery center of temecula aleve 500mg discount, and no significant distinction in survival is seen when comparing surgical bypass for palliation with nonsurgical drainage (Singhal et al, 2005). Endoscopic stenting for palliation is determined by the talent of the endoscopist, and initially, plastic stents may be inserted (see Chapter 29). Plastic stents had a mean patency of 126 days in one study (Davids et al, 1992), are cost-effective, and should C. Malignant Tumors Chapter 51A Extrahepatic bile duct tumors 831 be the first stenting modality used. In a singleinstitution retrospective trial of chemoradiation for 37 sufferers with unresectable cholangiocarcinoma, native management charges of 90% had been seen at 1 12 months and 71% at 2 years, whereas survival was 59% at 1 yr and 22% at 2 years (Ghafoori et al, 2011). No randomized potential multiinstitutional trials evaluating chemoradiation to other palliative modalities exist, and additional knowledge are wanted to confirm a definitive benefit from chemoradiation. First, a photosensitizing agent similar to porphyrin or -aminolevulinic acid is given intravenously and accumulates in cancer cells. Then, phototherapy delivered intraluminally to the tumor by cholangioscopy ends in activation and excitation of the photosensitizing agent, era of oxygen-free radicals, and tumor cell death, with a lower within the size of the tumor (Ortner, 2001). Systemic chemotherapy has been investigated for palliation of unresectable hilar cholangiocarcinoma. Median overall survival within the combination-chemotherapy group was considerably elevated compared with the single-agent group (11. Currently, the mixture of gemcitabine with cisplatin represents the usual of care in first-line chemotherapy for patients with regionally superior unresectable or metastatic biliary tract cancers. Clearly, nevertheless, more data and advances in chemotherapeutic brokers are wanted to improve the survival of patients with unresectable disease. Hilar cholangiocarcinoma represents a challenging illness process, and surgical resection offers sufferers the most effective alternative for long-term survival. Bergquist A, et al: Risk factors and medical presentation of hepatobiliary carcinoma in sufferers with major sclerosing cholangitis: a casecontrol study, Hepatology 27(2):311�316, 1998. Bergquist A, et al: Hepatic and extrahepatic malignancies in main sclerosing cholangitis, J Hepatol 36(3):321�327, 2002. Blechacz B, et al: Clinical diagnosis and staging of cholangiocarcinoma, Nat Rev Gastroenterol Hepatol 8(9):512�522, 2011. Borghero Y, et al: Extrahepatic bile duct adenocarcinoma: patients at high-risk for native recurrence treated with surgical procedure and adjuvant chemoradiation have an equal overall survival to patients with standard-risk treated with surgical procedure alone, Ann Surg Oncol 15(11):3147� 3156, 2008. Burak K, et al: Incidence and risk components for cholangiocarcinoma in primary sclerosing cholangitis, Am J Gastroenterol 99(3):523�526, 2004. Capussotti L, et al: Local surgical resection of hilar cholangiocarcinoma: is there nonetheless a spot Cherqui D, et al: Major liver resection for carcinoma in jaundiced patients with out preoperative biliary drainage, Arch Surg 135(3):302� 308, 2000. Dumitrascu T, et al: Resection for hilar cholangiocarcinoma: evaluation of prognostic elements and the impression of systemic inflammation on long-term outcome, J Gastrointest Surg 17(5):913�924, 2013. Endo I, et al: Clinical significance of intraoperative bile duct margin evaluation for hilar cholangiocarcinoma, Ann Surg Oncol 15(8):2104� 2112, 2008. Furusawa N, et al: Surgical remedy of one hundred forty four cases of hilar cholangiocarcinoma without liver-related mortality, World J Surg 38(5):1164� 1176, 2014. Giuliante F, et al: Liver resections for hilar cholangiocarcinoma, Eur Rev Med Pharmacol Sci 14(4):368�370, 2010. Gomez D, et al: Impact of specialised multi-disciplinary approach and an integrated pathway on outcomes in hilar cholangiocarcinoma, Eur J Surg Oncol 40(1):77�84, 2014. Hirano S, et al: Oncological benefit of preoperative endoscopic biliary drainage in patients with hilar cholangiocarcinoma, J Hepatobiliary Pancreat Sci 21(8):533�540, 2014. Igami T, et al: Surgical treatment of hilar cholangiocarcinoma in the "new period": the Nagoya University expertise, J Hepatobiliary Pancreat Sci 17(4):449�454, 2010. Ito F, et al: Resection of hilar cholangiocarcinoma: concomitant liver resection decreases hepatic recurrence, Ann Surg 248(2):273�279, 2008. Kobayashi A, et al: Disease recurrence patterns after R0 resection of hilar cholangiocarcinoma, Br J Surg 97(1):56�64, 2010. Li H, et al: Analysis of the surgical end result and prognostic elements for hilar cholangiocarcinoma: a Chinese experience, Dig Surg 28(3):226� 231, 2011. Matsuo K, et al: the Blumgart preoperative staging system for hilar cholangiocarcinoma: analysis of resectability and outcomes in 380 patients, J Am Coll Surg 215(3):343�355, 2012. Mizumoto R, Suzuki H: Surgical anatomy of the hepatic hilum with special reference to the caudate lobe, World J Surg 12(1):2�10, 1988. Nagahashi M, et al: Depth of invasion determines the postresectional prognosis for patients with T1 extrahepatic cholangiocarcinoma, Cancer 116(2):400�405, 2010. Nagino M, et al: Evolution of surgical therapy for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections, Ann Surg 258(1):129�140, 2013. Nakeeb A, et al: Cholangiocarcinoma: a spectrum of intrahepatic, perihilar, and distal tumors, Ann Surg 224(4):463�473, dialogue 473� 465, 1996. Neuhaus P, et al: Surgical administration of proximal bile duct cancer: prolonged right lobe resection increases resectability and radicality, Langenbecks Arch Surg 388(3):194�200, 2003. Neuhaus P, et al: Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma, Ann Surg Oncol 19(5): 1602�1608, 2012. Nuzzo G, et al: Improvement in perioperative and long-term consequence after surgical therapy of hilar cholangiocarcinoma: results of an Italian multicenter analysis of 440 patients, Arch Surg 147(1):26�34, 2012. Ono S, et al: Long-term outcomes after hepaticojejunostomy for choledochal cyst: a 10- to 27-year follow-up, J Pediatr Surg 45(2):376� 378, 2010. Ortner M: Photodynamic remedy for cholangiocarcinoma, J Hepatobiliary Pancreat Surg 8(2):137�139, 2001. Otto G, et al: Klatskin tumour: meticulous preoperative work-up and resection fee, Z Gastroenterol 49(4):436�442, 2011. Panjala C, et al: Impact of neoadjuvant chemoradiation on the tumor burden earlier than liver transplantation for unresectable cholangiocarcinoma, Liver Transpl 18(5):594�601, 2012. Paul A, et al: Klatskin tumors and the accuracy of the Bismuth-Corlette classification, Am Surg 77(12):1695�1699, 2011. Saini S: Imaging of the hepatobiliary tract, N Engl J Med 336(26):1889� 1894, 1997. Sakata J, et al: Catheter tract implantation metastases associated with percutaneous biliary drainage for extrahepatic cholangiocarcinoma, World J Gastroenterol 11(44):7024�7027, 2005. Saxena A, et al: Improved outcomes after aggressive surgical resection of hilar cholangiocarcinoma: a crucial analysis of recurrence and survival, Am J Surg 202(3):310�320, 2011. Singhal D, et al: Palliative management of hilar cholangiocarcinoma, Surg Oncol 14(2):59�74, 2005. Tamada K, et al: Endoscopic prognosis of extrahepatic bile duct carcinoma: Advances and present limitations, World J Clin Oncol 2(5): 203�216, 2011. Unno M, et al: Major hepatectomy for perihilar cholangiocarcinoma, J Hepatobiliary Pancreat Sci 17(4):463�469, 2010. Valle J, et al: Cisplatin plus gemcitabine versus gemcitabine for biliary tract most cancers, N Engl J Med 362(14):1273�1281, 2010.
Aleve: 500 mg, 250 mg
Cheap aleve 500 mg on-lineConsequently sciatica pain treatment natural buy 500mg aleve with mastercard, the medical management of a person affected person can be improved solely by contemplating all of the options of pancreatitis knee pain treatment uk buy cheap aleve 250mg on line. The first effort to classify and define pancreatitis by a worldwide group of experts led to the Marseille Consensus Meeting in 1963 (Sarles midsouth pain treatment center jobs generic 500mg aleve otc, 1965) pain management treatment options order 500 mg aleve with mastercard. The panel of pancreatologists agreed that acute and continual pancreatitis had been completely different diseases primarily because of totally different morphologic patterns. Relapsing pancreatitis was characterised by the presence of multiple episodes in a morphologic pattern of acute or continual processes. The distinctive options of the two ailments had been the pathologic benign course of acute irritation, with biologic restitution within the acute situation, and the progressively worsening parenchymal lesions in the persistent situation (Table 54. From the clinical perspective, acute and chronic pancreatitis show an analogous pattern, no much less than within the early phases. Progress within the comprehension of pancreatitis and its classification resulted from the Cambridge meeting (Sarner & Cotton, 1984). The importance of the clinical impact of various severity systemic responses was emphasized (Table fifty four. The Cambridge group identified the related problem of etiology, and the role of imaging in continual pancreatitis was addressed. In explicit, cholelithiasis and its issues lead to demonstrable alterations within the morphology of the duct of Wirsung, as said within the Cambridge classification (Buchler et al, 1987; Misra et al, 1990), and these morphologic changes may persist for many months. The rising consideration to duct morphology, and consequently to the cause-and-effect relationship of obstruction, resulted in new terminology at the second Marseille assembly held in 1984 (Singer et al, 1985). In addition to the traditional distinction between acute and persistent illness, a brand new entity was identified: obstructive persistent pancreatitis (Table 54. The function of duct obstruction within the chronic inflammatory process was acknowledged as a distinctive pathway to growing pancreatitis. This new idea has gained importance over time in distinguishing chronic calcifying pancreatitis, in alcoholics, from obstructive continual pancreatitis initially presenting as relapsing acute assaults owing to strictures resulting from different circumstances, such as solid tumors, mucinous plugs typical of intraductal papillary mucinous tumors, severe pancreatitis with duct disruption, and scar and irritation of the sphincter of Oddi of biliary origin. Regarding acute pancreatitis, one other hallmark was recognized by the second Marseille assembly: the absence of necrosis in gentle pancreatitis. A panel of experts met in Rome in 1988 to integrate the second Marseille classification into use (Table fifty four. The primary feature of the brand new classification (Sarles et al, 1989) was the assertion concerning the reversibility of the lesions noticed in the course of acute pancreatitis; even the extreme varieties confirmed complete scientific response in nearly half of extreme pancreatitis patients. In distinction, in persistent pancreatitis, some pathologic features have been defined as permanent, and the situation was described as persistent inflammatory pancreatitis, morphologically characterized by lack of exocrine parenchyma and fibrosis with mononuclear cell infiltration. For the first time, etiology specifically was addressed, with pancreas divisum and alcohol as attainable causes of acute pancreatitis. The want for further effort to higher define acute pancreatitis resulted from the observation that the terminology of the Rome assembly was conflicting and not widely applied worldwide (Lumsden & Bradley, 1990). In 1992, forty pancreatologists met in Atlanta and developed a model new, dependable classification system of acute pancreatitis (Table 54. The scientific and morphologic features of pancreatitis were considered, resulting in a dynamic ongoing classification system better in a place to characterize the individual affected person and predict disease severity. In 1997, a brand new definition of continual pancreatitis was published, dividing definite from possible continual pancreatitis (Table fifty four. This definition offered a listing of radiologic or laboratory options in persistent pancreatitis patients missing etiologic and pathogenetic options. The Manchester classification makes use of the phrases mild, average, and finish stage to symbolize disease development, allowing comparison between patient teams. In 2012, two main contributions had been revealed in the attempt to tackle the remaining medical questions. First, the Atlanta Classification of 1992 was updated via an international consensus (Banks et al, 2013). In this revised Atlanta Classification, a new severity classification is proposed along with a clear definition for diagnosing acute pancreatitis. Both interstitial and necrotizing pancreatitis are outlined, as properly as the person native issues. In particular, the Revised Atlanta Classification outlines the early and late phases of the disease, with the late part typically restricted to sufferers with moderate or extreme illness. Finally, severe acute pancreatitis is outlined solely by the presence of persistent organ failure, which is acknowledged as the main determinant of mortality. In the identical 12 months as the publication of the Revised Atlanta Classification, the determinant-based classification of acute pancreatitis severity was printed by a multidisciplinary panel of consultants (Dellinger et al, 2012). This classification makes use of persistent organ failure and infectious peripancreatic necrosis as determinants of mortality in acute pancreatitis, to classify sufferers into four categories (Table fifty four. Very recently, a number of studies have independently validated the 2 newer classifications and compared their performances relative to the unique Atlanta Classification of 1992 (AvcedoPiedra et al, 2014). Modified from Sarles H, et al, 1989: the classification of pancreatitis and definition of pancreatic disease. Modified from Homma T, et al, 1997: Diagnostic criteria for continual pancreatitis by the Japan Pancreas Society. Stage of subclinical chronic pancreatitis Nutritional elements Symptomatic persistent pancreatitis Hereditary elements I. Based on these features, the three types of continual pancreatitis are (1) particular continual pancreatitis, (2) possible continual pancreatitis, and (3) borderline persistent pancreatitis. Severe acute pancreatitis the Revised Atlanta Classification includes definitions of: acute peripancreatic fluid assortment, pancreatic pseudocyst, acute necrotic assortment, walled-off necrosis, infectious necrosis. Modified from Banks P, et al: Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. However, the Revised Atlanta Classification appears extra relevant within the day-to-day clinical care of patients. The classification systems will likely come full circle with the popularity of the deep however nonetheless controversial correlation between acute and chronic inflammation. As a take-home message for the scientific practice-the history of every patient have to be rigorously thought-about to determine danger components which will include alcohol abuse, obstruction, genetics, and autoimmune illness. The medical evidence of pancreasrelated stomach ache related to alterations of serum amylase and lipase led to the time period pancreatitis. Only the dynamic remark of patients with managed follow-up enables us to classify pancreatitis and to better define the illness, assigning the definitive labels supported by the biochemical and radiologic sources well characterized by the totally different classification methods obtainable. The clinician ought to acknowledge pancreatitis at an early stage however avoid assigning a "definitive" classification instantly, instead investigating all the components out there to decide whether a first acute attack may lead to continual changes with fibrosis, permanent disruptions, and exocrine endocrine insufficiency. Banks P, et al: Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by worldwide consensus, Gut 62:102�111, 2013. Bastid C, et al: Spontaneous healing of sclerosing cholangitis related to stricture of the main pancreatic duct, Pancreas 4:489�492, 1990. Epstein O, et al: the pancreas in major biliary cirrhosis and primary sclerosing cholangitis, Gastroenterology 83:1177�1182, 1982. Homma T, et al: Diagnostic criteria for chronic pancreatitis by the Japan Pancreas Society, Pancreas 15:14�15, 1997.
Syndromes - Sedation using medication called benzodiazepines until withdrawal is complete
- Serum creatinine
- Gastrointestinal tract
- MPS II, Hunter syndrome
- Masculine symptoms (virilization)
- Chronic thyroiditis
- Urinalysis
Buy 250 mg aleve fast deliverySome abscesses have inhomogeneous content material who pain treatment guidelines aleve 250 mg cheap, and if pus turns into thick pain treatment for arthritis in dogs buy aleve 250 mg on-line, the lesion may be confused with liver parenchyma lower back pain treatment exercise buy generic aleve 250mg online. During the arterial part pain treatment center of tempe buy aleve 500 mg amex, parenchyma surrounding the abscess might show segmental enhancement because of altered portal microcirculation in the infected tissue. It may provide details about portal vein patency and will demonstrate native issues that may include pleural effusion, vascular complications, and spontaneous rupture into the peritoneal cavity, retroperitoneum, and even the pericardium (Yang et al, 2004b). This may be necessary, for example, in a patient with polycystic liver illness and suspected an infection of a single lesion. In each circumstances, prior technetium-99m sulfur colloid scan offers extra diagnostic accuracy (Youssef et al, 2005). Single lesions are inclined to be cryptogenic, whereas a quantity of abscesses usually tend to have a biliary origin (Alvarez et al, 2001a and 2001b). Regardless of etiology, sufferers are mostly seen initially with a single lesion (Chan et al, 2005). In both single and a number of types, abscesses are extra frequently located in the right hepatic lobe, followed by a left and bilateral distribution (Chen et al, 2008a; Seeto & Rockey, 1996). Multiple microabscesses might current as broadly scattered lesions or with a cluster sample that tends to combination focally (Ralls, 2002). A 50-year-old affected person seen with fever, leukocytosis, and nonspecific abdominal pain. A, Computed tomographic scan confirmed an inflammatory process in the terminal ileum (arrow). B, A single pyogenic liver abscess within the portal section is located in the posterior section of the proper hepatic lobe (arrow). The cluster sample is usually related to coliform and enteric organisms and may occur in cholangitic abscesses secondary to biliary obstruction. Enterobacter cloacae Citrobacter freundii Gram-PositiveAerobes Streptococcus milleri Staphylococcus aureus Enterococcus spp. Identification of pathogens may be achieved by direct puncture of the abscess or by blood cultures. Moreover, unfavorable abscess cultures could additionally be found in 20% of sufferers (Lok et al, 2008). Poor tradition approach could be the purpose in some cases, however adverse cultures may additionally be caused by means of broad-spectrum antibiotics before cultures are obtained. Diabetes mellitus is sometimes recommended to be an important danger issue, however the pathogenesis continues to be unclear. Environmental or host elements could also be liable for the totally different incidence charges in Asia compared withWestern sequence (Cheng et al, 2002). The mechanisms of fuel formation entails combined acid fermentation of glucose, increased manufacturing of gasoline, impaired transportation of gasoline, and equilibrium between the gasoline in native tissues and that in abscesses (Lee et al, 2004). Modern imaging strategies allow accurate diagnosis, localization, and assessment of dimensions and actual variety of lesions. Abdominal imaging has changed surgical exploration as a diagnostic device, making potential the high success charges of the percutaneous approach. Nevertheless, remedy choices embody a large spectrum that ranges from antibiotic therapy alone to major operative interventions that would embody liver debridement and/or resection. Blood samples should be obtained earlier than beginning antibiotics, if potential, however not on the expense of therapy delay in an unstable patient. Liver Infection and Infestation Chapter seventy two Pyogenic liver abscess 1079 if current, and ought to be adjusted according to geographic variations and native antimicrobial treatment insurance policies. Empiric remedy of a cryptogenic abscess must be directed to cowl the most generally found organisms: gram-negative bacilli, anaerobes, and microaerophilic streptococci. A basic routine of ampicillin, an aminoglycoside, and metronidazole could additionally be a primary therapeutic approach. Other choices embody mixtures of third-generation cephalosporins or quinolones with metronidazole. Abscess secondary to acute cholangitis after biliary instrumentation and postoperative abscess after abdominal surgical procedure must be treated as nosocomial infections, with a definite epidemiology and flora in contrast with cryptogenic lesions. Imipenemcilastatin, vancomycin, and piperacillin-tazobactam therapies should be thought-about in these instances. A pattern culture, whenever possible, is necessary, and when info concerning the organism and antibiotic sensitivity turns into out there, modifications can be instituted. Criteria for medical stability include subjective and objective proof of enchancment in the inflammatory response produced by the an infection. The patient might then be switched to oral antibiotic remedy, perhaps even continued on an outpatient foundation for no much less than 2 more weeks. Drainage of all lesions is most likely not potential in sufferers with a number of small abscesses. If a biliary origin of those lesions is suspected, biliary decompression is obligatory, both by endoscopic, percutaneous, or surgical means (see Chapters 29, 30, and 42). The mortality charges reported in patients with a quantity of liver abscesses are high, ranging from 22% to 44%. Drainage of pus is often essential for an efficient resolution and to shorten the duration of antibiotic remedy, particularly in lesions larger than 5 cm in diameter. Multiple microabscesses (arrows) in a affected person after left colectomy on account of colon carcinoma. Fluoroscopy management and operating theaters under aseptic conditions are recommended. Local anesthesia and minimal sedation is used for most of those procedures (Giorgio et al, 2006). Controversy persists concerning the optimal process, significantly for small abscesses. Several nonrandomized research report experiences with each therapeutic approaches with good results. No vital differences have been present in length of hospitalization or procedure-related complication (Cai et al, 2014). The most necessary safety measure is to keep away from extreme manipulation of contaminated pus. Overdistension of the abscess with contrast brokers through the process and saline injections to wash the cavity are related to an increased danger of bacteremia and are subsequently not beneficial (Thomas et al, 2006). Flushing the catheter could additionally be helpful for maintaining its patency, particularly in cases of viscous pus. Furthermore, in such instances, larger catheters could additionally be wanted to drain the cavity efficiently. In some cases, after obvious successful drainage, imaging might present incomplete evacuation of the abscess cavity, and repositioning of the catheter, and even placement of additional catheters, could additionally be necessary.
Buy aleve 250mg low costFocusing on the extent of disease treating pain in dogs hips purchase 250 mg aleve with mastercard, some knowledge present that pancreatic resection ought to be prevented every time extrapancreatic illness is obvious if the results achieved in these sufferers in terms of progression-free and overall survival have been poor (Adler et al comprehensive pain headache treatment center derby ct buy aleve 250 mg on line, 2014) pain hypersensitivity treatment cheap aleve 500 mg line. If current medial knee pain treatment aleve 250mg generic, signs are just like those attribute of pancreatic adenocarcinoma, corresponding to 992 obstructive jaundice and higher digestive occlusion, fatigue, weight reduction, and stomach pain (see Chapter 62). Every main tumor can theoretically metastasize to the pancreas, and because of this, a personal medical history must be rigorously investigated and used to information the analysis. As mentioned earlier, most instances will present with multiple metastases in several organs, thus leading to a simple recognition of advanced illness. Whenever the pancreas is the single website of metastasis, the analysis may be more challenging. Only a couple of components may help to discriminate a main from a secondary pancreatic lesion, such as the most cancers antigen 19-9 serum level, which can be elevated in the case of metastatic illness when obstructive jaundice is current. From the morphologic standpoint, metastases to the pancreatic gland may have related features to the primary tumor. From Adler et al, 2014; Sperti et al, 2014; Sugimoto et al, 2013; and Tosoian et al, 2014. Few information are available that compare consequence between synchronous and metachronous metastases. In particular, it seems that metastasectomy for synchronous illness is associated with poorer prognosis, possibly due to undetected extrapancreatic metastatic sites. The scientific strategy in situations like these must be carefully weighed, considering the morbidity of a pancreatic resection performed on the time of major tumor surgery. Distal pancreatectomy should be performed at the time of primary tumor resection solely after a scientific preoperative staging, whereas head resections ought to usually be postponed. This multimodal therapy could give a twofold advantage: first, to management the tumor progress through the restoration from the primary tumor resection and second, to allow the detection of other metastatic sites in case of rapidly disseminating disease. This strategy ought to result in a better number of candidates for pancreatic head resection. However, the lower morbidity related to standard pancreatic resection over atypical resections (Bassi et al, 2003) could lead to the hypothesis that after a typical pancreatic resection is carried out, then a proper lymphadenectomy, as for the opposite pancreatic malignancies, should be achieved each time technically possible. Multiple lesions are common, and generally lesions may be radiographically occult. Because of this, each intraoperative gland palpation and ultrasound examination ought to be carried out and might reveal nodules that had not been preoperatively detected by commonplace imaging (Zerbi et al, 2008). Moreover, an correct pathology examination might determine occult nodules in the resected specimen. On the opposite hand, in the light of the fact that many of these lesions are sluggish rising with a low probability of lymph node metastases, enucleation or partial pancreatic resection could additionally be pursued. However, most authors choose to carry out standard pancreatic resections, even in instances of small pancreatic metastases (Adler et al, 2014). The advantages of normal procedures embrace achieving a whole lymphadenectomy and reducing local recurrence and probably postoperative complication rates. For sufferers with a quantity of lesions, to carry out a standard resection along with enucleation in an effort to keep away from complete pancreatectomy seems to be feasible. However, long-term follow-up should be scheduled for the potential of local relapse within the pancreas, as properly as in other distant organs. Data for these variants are too restricted to define proper biology and pure history. Whenever different organs are involved, pancreatic resections are related to very poor outcome with early relapse and demise (Reddy & Wolfgang, 2009; Strobel et al, 2009; Sugimoto et al, 2013). In such chosen instances, the surgeon should be conscious of the poor consequence after surgical procedure, and the clinical determination must be taken solely in the setting of a multidisciplinary strategy. Such oncologic analysis has been already assessed for liver metastases of colorectal origin (Pulitano et al, 2010; Tomlinson et al, 2007). Unfortunately, there are sparse data available on the long-term end result after resection of pancreatic metastases (Table 64. In our experience, the median total survival of a cohort of resected sufferers was a hundred and forty months (95% confidence interval, a hundred and one. From Facy et al, 2013; Konstantinidis et al, 2010; Law et al, 2003; Strobel et al, 2009; Tosoian et al, 2014; and Zerbi et al, 2008. This is notably better than the outcome obtained within the cited Italian multicenter examine for the subgroup of medically treated sufferers (median total survival of 86 months). Nevertheless, the actual good factor about resection ought to be evaluated only in the mild of the long-term results. We have found a really favorable 25% disease-free survival 10 years after resection, which emphasizes that only a healing resection has the flexibility to provide long-term disease-free survival. In the fashionable era, and as for different oncologic illness, a multidisciplinary approach involving surgeons and medical oncologists ought to be advocated to "tailor" the appropriate remedy for the single affected person. Pan B, et al: Secondary tumors of the pancreas: a case sequence, Anticancer Res 32:1449�1452, 2012. Perez Ochoa A, et al: Pancreatic metastases from ductal and lobular carcinomas of the breast, Clin Transl Oncol 9:603�605, 2007. Reddy S, et al: Pancreatic resection of isolated metastases from nonpancreatic main cancers, Ann Surg Oncol 15:3199�3206, 2008. Sperti C, et al: Metastatic tumors to the pancreas: the position of surgery, World J Gastrointest Oncol 6:381�392, 2014. Strobel O, et al: Survival data justifies resection for pancreatic metastases, Ann Surg Oncol 16:3340�3349, 2009. Sugimoto M, et al: Pancreatic resection for metastatic melanoma originating from the nasal cavity: a case report and literature evaluation, Anticancer Res 33:567�573, 2013. Yamamoto H, et al: Surgical remedy for pancreatic metastasis from soft-tissue sarcoma: report of two circumstances, Am J Clin Oncol 24:198� 200, 2001. Zerbi A, et al: Pancreatic metastasis from renal cell carcinoma: which sufferers benefit from surgical resection Akashi Y, et al: Outcome after surgical resection of isolated metastases to the pancreas, Hepatogastroenterology 57:1549�1552, 2010. Balzano G, et al: Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy, Br J Surg 95:357�362, 2008. Bassi C, et al: High recurrence rate after atypical resection for pancreatic metastases from renal cell carcinoma, Br J Surg ninety:555�559, 2003. Bednar F, et al: Breast most cancers metastases to the pancreas, J Gastrointest Surg 17:1826�1831, 2013. Crippa S, et al: Surgical remedy of metastatic tumors to the pancreas: a single center expertise and evaluation of the literature, World J Surg 30:1536�1542, 2006. Facy O, et al: Interest of intraoperative ultrasonography throughout pancreatectomy for metastatic renal cell carcinoma, Clin Res Hepatol Gastroenterol 37:530�534, 2013. Ghavamian R, et al: Renal cell carcinoma metastatic to the pancreas: medical and radiological options, Mayo Clin Proc seventy five:581�585, 2000. Jarufe N, et al: Surgical therapy of metastases to the pancreas, Surgeon 3:79�83, 2005. Jingu K, et al: Surgical treatment of a solitary pancreatic metastasis from renal cell carcinoma: report of a case, Surg Today 28:91�94, 1998.

Buy cheap aleve 500mg on-lineAloia T back pain treatment nyc purchase aleve 250mg overnight delivery, et al: Venous thromboembolism prophylaxis in liver surgical procedure pain medication for dogs after neuter order 500 mg aleve free shipping, J Gastrointest Surg 20(1):221�229 heel pain treatment youtube order aleve 500mg fast delivery, 2016 knee pain treatment urdu cheap aleve 250 mg. Assumpcao L, et al: Patterns of recurrence following liver resection for colorectal metastases: effect of primary rectal tumor site, Arch Surg 143(8):743�749, discussion 749�750, 2008. Balzan S, et al: the "50-50 standards" on postoperative day 5: an correct predictor of liver failure and demise after hepatectomy, Ann Surg 242(6):824�828, dialogue 828�829, 2005. Belli G, et al: Liver resection for hepatic metastases: 15 years of expertise, J Hepatobiliary Pancreat Surg 9(5):607�613, 2002. Cunningham D, et al: Randomised trial of irinotecan plus supportive care versus supportive care alone after fluorouracil failure for patients with metastatic colorectal cancer, Lancet 352(9138):1413�1418, 1998. Cunningham D, et al: Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal most cancers, N Engl J Med 351(4):337�345, 2004. De Gramont A, et al: Randomized trial evaluating month-to-month low-dose leucovorin and fluorouracil bolus with bimonthly high-dose leucovorin and fluorouracil bolus plus steady infusion for advanced colorectal cancer: a French intergroup research, J Clin Oncol 15(2):808� 815, 1997. De Gramont A, et al: Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer, J Clin Oncol 18(16):2938�2947, 2000. Doci R, et al: One hundred patients with hepatic metastases from colorectal cancer treated by resection: analysis of prognostic determinants, Br J Surg 78(7):797�801, 1991. Ekberg H, et al: Pattern of recurrence in liver resection for colorectal secondaries, World J Surg 11(4):541�547, 1987. Elias D, et al: Outcome of posthepatectomy-missing colorectal liver metastases after complete response to chemotherapy: impact of adjuvant intra-arterial hepatic oxaliplatin, Ann Surg Oncol 14(11):3188� 3194, 2007. Findlay M, et al: Noninvasive monitoring of tumor metabolism utilizing fluorodeoxyglucose and positron emission tomography in colorectal most cancers liver metastases: correlation with tumor response to fluorouracil, J Clin Oncol 14(3):700�708, 1996. Floriani I, et al: Performance of imaging modalities in the prognosis of hepatocellular carcinoma: a systematic review and meta-analysis, Ultraschall Med 34(5):454�462, 2013. Fong Y, et al: Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: evaluation of 1001 consecutive instances, Ann Surg 230(3):309�318, 1999. Fong Y, et al: Long-term survival is superior after resection for most cancers in high-volume centers, Ann Surg 242(4):540�547, 2005. Giacchetti S, et al: Long-term survival of sufferers with unresectable colorectal cancer liver metastases following infusional chemotherapy with 5-fluorouracil, leucovorin, oxaliplatin and surgical procedure, Ann Oncol 10(6):663�669, 1999. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, Chest 141(Suppl 2):e227S�e277S, 2012. Hagness M, et al: Liver transplantation for nonresectable liver metastases from colorectal cancer, Ann Surg 257(5):800�806, 2013. Ito H, et al: Effect of postoperative morbidity on long-term survival after hepatic resection for metastatic colorectal cancer, Ann Surg 247(6):994�1002, 2008. Ito K, et al: Surgical treatment of hepatic colorectal metastasis: evolving position in the setting of enhancing systemic therapies and ablative remedies in the 21st century, Cancer J 16(2):103�110, 2010. Iwatsuki S, et al: Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system, J Am Coll Surg 189(3):291�299, 1999. Jaeck D, et al: One or two-stage hepatectomy mixed with portal vein embolization for initially nonresectable colorectal liver metastases, Am J Surg 185(3):221�229, 2003. Karoui M, et al: Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases, Ann Surg 243(1): 1�7, 2006. Kato T, et al: Therapeutic outcomes for hepatic metastasis of colorectal most cancers with special reference to effectiveness of hepatectomy: analysis of prognostic elements for 763 instances recorded at 18 institutions, Dis Colon Rectum 46(10):S22�S31, 2003. P: Determinants of long-term survival after major surgery and the adverse impact of postoperative issues, Ann Surg 242(3):326�341, discussion 341�343, 2005. Knosel T, et al: Chromosomal alterations throughout lymphatic and liver metastasis formation of colorectal most cancers, Neoplasia 6(1):23�28, 2004. Kokudo N, et al: Genetic and histological assessment of surgical margins in resected liver metastases from colorectal carcinoma: minimum surgical margins for profitable resection, Arch Surg 137(7):833�840, 2002. Kopetz S, et al: Improved survival in metastatic colorectal most cancers is related to adoption of hepatic resection and improved chemotherapy, J Clin Oncol 27(22):3677�3683, 2009. Leen E, et al: Potential value of contrast-enhanced intraoperative ultrasonography during partial hepatectomy for metastases: an important investigation before resection Machi J, et al: Intraoperative ultrasonography in screening for liver metastases from colorectal most cancers: comparative accuracy with traditional procedures, Surgery 101(6):678�684, 1987. Mala T, et al: A comparative study of the short-term end result following open and laparoscopic liver resection of colorectal metastases, Surg Endosc 16(7):1059�1063, 2002. Martin R, et al: Simultaneous liver and colorectal resections are protected for synchronous colorectal liver metastasis, J Am Coll Surg 197(2): 233�241, 2003. Mentha G, et al: Neoadjuvant chemotherapy and resection of superior synchronous liver metastases earlier than therapy of the colorectal main, Br J Surg 93(7):872�878, 2006. Miller G, et al: Outcomes after resection of synchronous or metachronous hepatic and pulmonary colorectal metastases, J Am Coll Surg 205(2):231�238, 2007. Minagawa M, et al: Extension of the frontiers of surgical indications within the therapy of liver metastases from colorectal cancer: long-term results, Ann Surg 231(4):487�499, 2000. Mise Y, et al: Ninety-day postoperative mortality is a legitimate measure of hepatopancreatobiliary surgical quality, Ann Surg 62(6):1071� 1078, 2015. Mitry E, et al: Adjuvant chemotherapy after doubtlessly healing resection of metastases from colorectal most cancers: a pooled evaluation of two randomized trials, J Clin Oncol 26(30):4906�4911, 2008. Nikfarjam M, et al: Survival outcomes of sufferers with colorectal liver metastases following hepatic resection or ablation in the era of efficient chemotherapy, Ann Surg Oncol 16(7):1860�1867, 2009. Nordlinger B, et al: Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, primarily based on 1568 patients. Nordlinger B, et al: Hepatic resection for colorectal liver metastases: influence on survival of preoperative components and surgical procedure for recurrences in 80 patients, Ann Surg 205(3):256�263, 1987.
[newline]Norstein J, Silen W: Natural history of liver metastases from colorectal carcinoma, J Gastrointest Surg 1(5):398�407, 1997. Nuzzo G, et al: Influence of surgical margin on sort of recurrence after liver resection for colorectal metastases: a single-center expertise, Surgery 143(3):384�393, 2008. Parks R, et al: Adjuvant chemotherapy improves survival after resection of hepatic colorectal metastases: evaluation of data from two continents, J Am Coll Surg 204(5):753�761, discussion 761�763, 2007. Petrowsky H, et al: Second liver resections are protected and effective remedy for recurrent hepatic metastases from colorectal most cancers: a bi-institutional evaluation, Ann Surg 235(6):863�871, 2002. Pozzo C, et al: Neoadjuvant remedy of unresectable liver disease with irinotecan and 5-fluorouracil plus folinic acid in colorectal cancer sufferers, Ann Oncol 15(6):933�939, 2004. Rougier P, et al: Prospective examine of prognostic factors in patients with unresected hepatic metastases from colorectal most cancers. Rubbia-Brandt L, et al: Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in sufferers with metastatic colorectal cancer, Ann Oncol 15(3):460�466, 2004. Scheele J, et al: Hepatic metastases from colorectal carcinoma: impression of surgical resection on the pure historical past, Br J Surg 77(11):1241� 1246, 1990. Schlag P, et al: Resection of liver metastases in colorectal cancer: aggressive evaluation of remedy results in synchronous versus metachronous metastases, Eur J Surg Oncol 16(4):360�365, 1990. Shindoh J, et al: Optimal morphologic response to preoperative chemotherapy: an alternate end result end point earlier than resection of hepatic colorectal metastases, J Clin Oncol 30(36):4566�4572, 2012.
Buy 250mg aleve visaProper identification of margins and their adequate sampling are important components in the pathologic evaluation of a pancreatoduodenectomy specimen (Adsay et al swedish edmonds pain treatment center aleve 250 mg discount, 2012 pain treatment guidelines 2012 purchase 500mg aleve mastercard, 2014; Esposito et al pacific pain treatment center victoria generic aleve 250mg without prescription, 2008; Ferrone et al regional pain treatment center discount aleve 250 mg fast delivery, 2008; Schlitter & Esposito, 2010); nevertheless, what constitutes a margin stays controversial (Adsay et al, 2014). For instance, the anterior surfaces are regarded as a margin by some but not by others. Similarly, whether or not to think about the posterior free surfaces of the pancreas (partly similar to vena cava surface) as a margin has also been highly controversial, with vastly different views by completely different authors. Readers are referred to a latest evaluation article for detailed analysis of this subject (Adsay et al, 2014). As anticipated, ductal adenocarcinoma exhibits immunohistochemical proof of ductal differentiation. Substantial developments have occurred in understanding the molecular carcinogenesis of ductal adenocarcinoma (see Chapter 9B). Mutation of p16 or methylation of the promoter also is frequent (>80%) and represents the pathogenetic link with the familial atypical a quantity of mole�melanoma syndrome (Hruban et al, 2001a). The latter seems to have a modest degree of specificity for pancreatic ductal adenocarcinoma. Fanconi anemia gene alterations even have been recognized (van der Heijden et al, 2003). Abnormalities in mismatch restore proteins and microsatellite instability are uncommon, though pancreatic ductal adenocarcinomas can occur as one of the less frequent manifestations of Lynch syndrome. Replacement of the normal cuboidal, nonmucinous ductal epithelium with columnar cells that contain plentiful apical mucin, however without architectural complexity. As the intraductal neoplasm progresses, it acquires extra papillary structure and cytologic atypia. Other Invasive Carcinomas Related to Ductal Adenocarcinoma Certain types of carcinomas are carefully related to , and often seen in association with, ductal adenocarcinoma (Klimstra & Adsay, 2009). Undifferentiated carcinoma could be thought to be the least differentiated form of ductal adenocarcinoma, in which attribute tubule formation is now not evident or solely focal. Undifferentiated carcinomas embody sarcomatoid (spindle cell) carcinoma, anaplastic large cell carcinoma, and carcinosarcoma. Rarely, the sarcomatoid elements of those tumors may show aberrant differentiation, together with bone and cartilage formation. Studies have shown that the osteoclastic big cells are nonneoplastic histiocytic cells (Westra et al. The true neoplastic cells in this tumor sort are the sarcomatoid mononuclear cells. Undifferentiated carcinomas with osteoclast-like giant cells usually appear properly demarcated and kind a large solitary mass and exhibit nodular, pushing-border infiltration. If examined rigorously, many such tumors seem to have substantial intraductal development. These are clearly malignant neoplasms, most exhibiting an aggressive clinical course; however, some examples with minimal ductal adenocarcinoma elements have a protracted clinical course. In a current examine, many of those patients skilled unexpectedly long survival, with an general 5-year survival of 42% (Muraki et al, 2016). Squamous cell carcinoma and adenosquamous carcinoma of this region are extremely aggressive tumors (Kardon et al, 2001), with a prognosis that could be worse than that of typical ductal adenocarcinoma. Medullary carcinomas seem to be considerably extra common in the ampulla and duodenum than in the pancreas, and therefore, earlier than a case may be categorised as pancreatic, these potentialities must be excluded. Syncytial nodules of large, poorly differentiated epithelioid cells with a pushing pattern of invasion characterize medullary carcinomas. Goggins and colleagues (1998) found that these tumors have a extra protracted medical course, however further information are essential to outline the prognosis of those uncommon tumors. Intraductal Neoplasms Intraductal neoplasms constitute an increasingly encountered and necessary category of pancreatic tumors of ductal origin, characterized by intraductal polypoid, papillary nodules that are often related to cystic dilation of the ducts (Adsay et al, 2010, 2016; Basturk et al, 2009). Such lesions at the moment are also termed tumoral intraepithelial neoplasia (Adsay et al, 2015; Tanaka et al, 2006). It is estimated that about 15% of invasive adenocarcinomas within the pancreas come up from these tumor types. The neoplasms included under this umbrella of "intraductal tumors" are intraductal papillary mucinous neoplasms and intraductal tubulopapillary neoplasms. Radiographic findings of ductal dilation with irregularities additionally are sometimes diagnostic. As the biology of these tumors was higher understood, and higher management protocols have been devised, it grew to become clear that a two-tiered system is extra meaningful and applicable. Tumors composed nearly exclusively of the colloid pattern-in which the mucin/epithelium ratio may be very excessive, and most carcinoma cells are floating inside the mucin (detached from the stroma)-have a unique biology with an unusually protracted medical course (Hruban et al, 2007; Seidel et al, 2002). Anecdotal proof means that open biopsy of colloid carcinomas could contribute to dissemination, presumably because of the adherent nature of the mucin. Colloid carcinomas also are inclined to be larger and better demarcated than ductal adenocarcinomas, and their molecular alterations seem to be somewhat distinctive. Overall, colloid carcinomas have a considerably higher prognosis than ductal adenocarcinomas, with 5-year survival greater than 55% (Adsay et al, 2001; Marchegiani et al, 2015b; Winter et al, 2015). The papillae resemble these of a villous adenoma of the large bowel, with pseudostratified, elongated nuclei with apical mucinous cytoplasm. This is very pertinent to management of these tumors, as a result of as beforehand discussed, colloid carcinomas not only have a means more protracted scientific course, but also may be nearer in biology to intestinal adenocarcinomas than pancreatic. In reality, despite their large dimension and complexity, extraordinarily low (if any) mortality has been attributed to this tumor kind. They seem to be not solely precursors but also "markers" of invasive adenocarcinoma. Patients with high-grade dysplasia on occasion may expertise recurrences and metastases (White et al, 2007), presumably the result of undetected foci of invasive carcinoma; invasive carcinoma has a malignant clinical course, although typically considerably more protracted than that of odd ductal adenocarcinoma. Intraductal Tubulopapillary Neoplasms Intraductal tubulopapillary neoplasm is a recently acknowledged category of mass-forming (>1. It is a rare tumor seen at an average age of 53 years, and it presents with nonspecific signs. Intraductal tubulopapillary neoplasm happens predominantly in the head of the pancreas but might involve any half. The common attribute current in all circumstances is intraductal nodular, polypoid development of spherical, cuboidal nonmucinous cells in a tubular, or every so often, tubulopapillary association. Tubules are small to medium sized, sometimes properly fashioned, with recognizable lumina of variable sizes, although extra poorly outlined, abortive tubular arrangements can be seen in some cases. Mitotic activity is commonly high, and one third of instances have invasive carcinoma of the tubular sort. Invasion, usually microscopic, is troublesome to assess in these tumors due to the relative complexity of the intraductal part. Limited follow-up means that these are indolent neoplasms with a protracted clinical course. A variety of pancreatic neoplasms can present outstanding intraductal development, together with acinar cell carcinomas (Ban et al, 2010; Basturk et al, 2007), pancreatic neuroendocrine tumors, osteoclastic giant cell carcinomas (Muraki et al, 2016), and even metastatic tumors, and thus fall into the differential diagnosis of these intraductal neoplasms.
Discount aleve 250 mg otcThe symptoms that bring these malignancies to medical consideration range based upon the location of the tumor inside the pancreas and the stage at presentation shoulder pain treatment options discount 500 mg aleve. The majority of resectable pancreas cancers happen in the best facet of the pancreas treatment for long term pain from shingles safe aleve 500 mg, within the head pain treatment program johns hopkins generic aleve 250mg on line, or uncinate means of the gland pain treatment ulcerative colitis order aleve 500 mg on line. Classic signs from these right-sided tumors include jaundice from biliary obstruction, usually accompanied by pruritus, and epigastric ache radiating to the again from tumor involvement of the celiac plexus. Additionally, pancreatitis in the absence of cholelithiasis or ethanol abuse ought to arouse suspicion for cancer in sufferers age 60 years or older. For such left-sided tumors, ache is the most typical presenting symptom, occasionally steatorrhea may be seen, and jaundice is rare. Nausea, anorexia, weight reduction, and fatigue are commonly reported and often are present for a while earlier than analysis. Because of the generalized and customary nature of these symptoms, they rarely lead directly to a analysis except they turn into profound. Typically, jaundice is the only bodily finding in "early"stage pancreatic cancer. The basic physical findings of left supraclavicular adenopathy (Virchow node), periumbilical adenopathy (Sister Mary Joseph node), or a agency circumferential rim of tumor at the top of the rectum on digital rectal examination (Blumer shelf from drop metastases) are discovered only with advanced, disseminated illness. Less particular findings that additionally sometimes indicate advanced disease include temporal losing, ascites, hepatomegaly from metastatic disease, or a palpable stomach mass. Elevated liver function checks are nonspecific and require both further serologic testing and imaging to investigate their etiology. However, such new-onset diabetes has a low sensitivity and specificity for the analysis of pancreatic cancer, and vital overlap is discovered between the typical age of onset of diabetes mellitus and pancreatic most cancers. The incidence of diabetes mellitus can additionally be much greater than that of pancreatic most cancers, additional limiting its utility as a diagnostic sign. Ongoing analysis has produced many potential diagnostic biomarkers for pancreatic most cancers (Harsha et al, 2009; Winter et al, 2013). The proportion of pancreatic cancer sufferers who fall into this group has been reported to range from 10% to 34% (Berger et al, 2008; Tempero et al, 1987). However, promising analysis to discover different diagnostic, prognostic, and predictive biomarkers is ongoing (Winter et al, 2013). These modalities will suggest processes in the pancreas that require applicable further analysis. Water is given orally, as a end result of oral contrast within the abdomen or duodenum could cause a streak artifact that limits visualization of the pancreas and subsequent 3D image rendering. Such scans usually show the tumor as a low-density (hypodense) lesion within the pancreas, greatest seen during the arterial phase of contrast enhancement. The venous phase of contrast enhancement is useful to evaluate distant (mainly liver) metastases, and regional lymphadenopathy (Raman et al, 2012). However, the routine placement of a biliary endoprosthesis for all jaundiced sufferers without cholangitis ought to be discouraged. Multiple research have shown a doubling of the wound an infection danger and a slight enhance in overall complication threat with preoperative biliary stenting (Pisters et al, 2001a; Sohn et al, 2000). For most sufferers seen initially with a pancreatic mass and jaundice, early attempt at operative resection is preferable to endoscopic biliary stenting and delayed surgical resection (Kennedy et al, 2010). Reported sensitivities for the diagnosis of pancreatic neoplasia have ranged from 69% to 94%. This can be of nice profit to unresectable or borderline resectable sufferers who need a confirmed tissue diagnosis before the initiation of chemotherapy. Pancreatic biopsy ought to be reserved for sufferers with regionally unresectable or metastatic disease or for these clinical situations by which a true diagnostic or management dilemma is present or when neoadjuvant therapy is taken into account. Such situations would come with sufferers with a history of different cancers with a sensible likelihood of a metastasis to the periampullary region (renal cell cancer, melanoma), sufferers with a suspicion for autoimmune pancreatitis, or patients with marginal physiologic reserves at prohibitive risk for surgical intervention. When preoperative imaging means that autoimmune pancreatitis (see Chapters 18, 57, and 59) could additionally be current, IgG4 ranges also wants to be obtained, as a end result of elevated IgG4 is very particular for this process. In the presence of suspected metastatic disease, biopsy of the distant lesion, if accessible, is most well-liked versus biopsy of the primary pancreatic lesion. Classic T, N, and M parameters are used for tumor dimension, nodal involvement, and distant metastases, but stage grouping is carried out in accordance with surgical resectability. Resectable pancreatic adenocarcinoma in the head and uncinate process, showing well-preserved fats plane (arrow) between tumor (T) and superior mesenteric artery (A). Modern cross-sectional imaging has lowered that rate considerably, as mentioned earlier. Disagreement exists in the literature about the role of staging laparoscopy within the analysis of patients with radiographically resectable pancreatic cancer. Unresectable pancreatic adenocarcinoma in the head and uncinate course of, showing lack of fat airplane (arrow) between tumor (T) and superior mesenteric artery (A). A metallic endoprosthesis is seen as a circular construction in the distal frequent bile duct. Taking the data as an entire, staging laparoscopy seems greatest reserved for choose sufferers in whom an elevated chance of intraabdominal dissemination exists. This dedication must be made in consultation with an professional in pancreatic surgery. Surgical resection of pancreatic most cancers remains the one doubtlessly healing therapy. Malignant Tumors Chapter 62 Pancreatic most cancers: medical elements, assessment, and management 983 to 30%) diagnosed with pancreatic most cancers are candidates for curative resection on the time of prognosis. The reason for this extremely low survival in patients who introduced with localized most cancers is unclear, as even patients with domestically unresectable tumors expertise higher median illness particular outcomes. More recently, Raigani and colleagues (2014) confirmed the nonetheless alarmingly low surgical resection charges, 36% to 63%, for stage 1 and a pair of pancreatic cancers, respectively. This represents a gross underutilization of surgical intervention for potentially curable pancreatic cancer within the United States, which the authors postulate could additionally be because of a nihilistic perspective toward pancreatic most cancers care. At our institution, the use of a sophisticated recovery pathway, fluid restriction protocols, discharge planning, and postoperative exercise regimens have improved the perioperative outcomes and restoration of our patients (Kennedy et al, 2007; Lavu et al, 2014; Yeo et al, 2012). Results Recurrent controversies have endured over the effectiveness of surgical resection for pancreatic cancer (Crile, 1970; Gudjonsson, 1995). The preponderance of latest information which have emerged from giant specialised centers refute previous claims of futility and lack of long-term survival. A publication in 2006 by Riall and colleagues examined the precise 5 12 months survival rates after pancreaticoduodenectomy, all phases combined, for pancreatic and periampullary cancer and reported actuarial 10 12 months survival. This analysis included a positive lymph node rate of 48% and a constructive margin rate of 8% within the total periampullary cohort. A comparable examine by Ferrone and colleagues (2008) revealed an actual 5-year survival fee of 23% for resected stage Ia disease, and all-stage actual 5 12 months and 10 yr survival rates of 12% and 5%, respectively, have been reported. This group just lately up to date these knowledge with an precise 5 yr survival price of 19% and a 10 yr survival rate of 10%. They found that the numerous clinicopathologic factors predicting 5 and 10 year survival had been adverse surgical margins and negative nodal standing; nonetheless, apparently, 41% of long-term survivors had constructive lymph nodes, and 24% had a constructive surgical margin (Ferrone et al, 2012).
References - Hendrix SL, McNeeley SG: Effect of selective estrogen receptor modulators on reproductive tissues other than endometrium, Ann N Y Acad Sci 949:243, 2001.
- Martinez JJ: Type 1 pilus-mediated bacterial invasion of the bladder epithelial cells, EMBO J 19:2803-2812, 2000.
- Xu J, Zheng SL, Isaacs SD, et al: Inherited genetic variant predisposes to aggressive but not indolent prostate cancer, Proc Natl Acad Sci 107:2136n2140, 2010.
- Westland R, Schreuder MF, Bokenkamp A, et al: Renal injury in children with a solitary functioning kidneyothe KIMONO study, Nephrol Dial Transplant 26(5):1533n1541, 2011.
- Brumback BG, Wade CD. Simultaneous rapid culture for four respiratory viruses in the same cell monolayer using a differential multicolored fluorescent confirmatory stain. J Clin Microbiol. 1996;34: 798-801.
|