Colchisol
William G. Gossman, M.D. - Assistant Professor
- Finch University/Chicago Medical School
- Project Medical Director
- Mount Sinai Hospital
- Chicago, IL
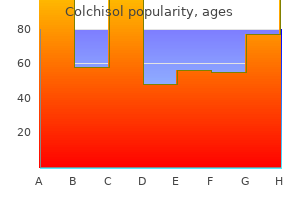
Colchisol 0.5mg without a prescriptionA permanent suture is initially passed by way of one uterosacral ligament as high as possible antibiotics korean generic 0.5mg colchisol amex. Successive bites at 1- to 2-cm intervals then are taken via the anterior serosa of the bowel antibiotics for strep throat cheap colchisol 0.5 mg without a prescription, till the opposite uterosacral ligament is reached antibiotic resistance transfer order 0.5 mg colchisol with amex. This suture is left untied antibiotic before surgery discount 0.5mg colchisol with mastercard, and successive identical sutures are positioned as wanted, progressing toward the posterior vaginal cuff. The variety of inner McCall sutures positioned depends on the scale and depth of the enterocele or cul-de-sac. After all of the internal everlasting sutures have been positioned and their ends held laterally with out tying, one or two delayed absorbable No. These are inserted from the vaginal lumen slightly below the middle of the minimize fringe of the posterior vaginal cuff, through the peritoneum, and thru the best uterosacral ligament. As described in step 2, successive bites are taken across the cul-de-sac and into the left uterosacral ligament. This suture is handed through the peritoneum and vaginal epithelium, adjacent to the purpose of entry. Finally, the delayed absorbable sutures are tied in a fashion that brings the posterior vagina up to the extent of the uterosacral ligaments. A, the cul-de-sac is digitally palpated, and extreme peritoneum and posterior vaginal wall are noted. B, A wedge of tissue (dotted line), which incorporates full-thickness vaginal wall and peritoneum, is excised to lower the caliber of the higher portion of the posterior vaginal wall. D, Tying these sutures obliterates the cul-de-sac, helps the vaginal cuff, and increases posterior vaginal wall length. The remnants of the uterosacral ligaments are discovered posterior and medial to the ischial spine, and the ureter can generally be palpated or visualized alongside the pelvic aspect wall, anywhere from 2 to 5 cm ventral and lateral to the ischial spine. One end of the Allis clamp must be intraperitoneal and the opposite in the lumen of the vagina. Usually, two to three delayed absorbable sutures are handed by way of the ligament on all sides. In conditions the place the cul-de-sac could be very deep and broad, inner McCall-type sutures may be positioned, plicating the distal remnants of the uterosacral ligaments across the midline. Cystoscopy after intravenous injection of indigo carmine is recommended to document bilateral ureteral patency. The sacrospinous ligaments extend from the ischial spines on all sides to the decrease portion of the sacrum and coccyx. A, probably the most distinguished portion of the prolapsed vaginal vault is grasped with Allis clamps. The retractor lifts the sponges up out of the lower pelvis, thus completely exposing the cul-de-sac. When applicable downward traction is applied on the uterosacral ligaments with an Allis clamp, the uterosacral ligaments are simply palpated bilaterally. D, Delayed absorbable sutures are handed through the uppermost portion of the uterosacral ligaments on each side and are individually tagged. E, Each end of the beforehand handed sutures is brought out through the posterior peritoneum and the posterior vaginal wall. A free needle is used to move both ends of those delayed absorbable sutures via the full thickness of the vaginal wall. F, the anterior colporrhaphy is begun by initiating a dissection between the prolapsed bladder and the anterior vaginal wall. The fibromuscular coccygeus is attached directly to the underlying sacrotuberous ligament. Also, an plentiful vascular provide that includes inferior gluteal vessels and hypogastric venous plexus lies superiorly. The sacrospinous ligament colpopexy is completed for average to severe apical prolapse after hysterectomy; it can additionally be accomplished with simultaneous vaginal hysterectomy or even as a hysteropexy (see Chapter 26). H, the vagina has been appropriately trimmed and closed with interrupted or steady delayed absorbable sutures. After closing the vagina, the delayed absorbable sutures that had been previously brought out by way of the total thickness of the posterior vaginal wall are tied, thereby elevating the prolapsed vaginal vault high up into the hole of the sacrum. A, the uterosacral ligament at in regards to the level of the ischial spine is grasped with an Allis clamp. B, Three sutures are positioned through the ipsilateral uterosacral ligament after which via the vaginal apex. This operation usually requires simultaneous correction of the anterior and posterior vaginal partitions and an enterocele repair. Placing the prolapsed vaginal apex to the sacrospinous ligament to see whether or not the vagina is lengthy enough to complete the repair and whether the anterior and posterior vaginal wall prolapse disappear helps to determine whether cystocele and rectocele repairs are wanted. If the uterus is present, a vaginal hysterectomy is done and the peritoneum is closed, as previously described. Sacrospinous cervicopexy or hysteropexy is also carried out utilizing comparable approach, if desired (see Chapter 26). The apex of the vagina is grasped with two Allis clamps, and downward traction is used to decide the extent of the vaginal prolapse and associated vaginal support defects. The vaginal apex then is decreased to the sacrospinous ligament intended to be used. In the posterior approach a midline posterior vaginal wall incision is made simply in need of the apex of the vagina, leaving a small vaginal bridge approximately 3 or four cm extensive. The perirectal space or the space along the peritoneum close to the apex then is entered by breaking through the fibroareolar tissue simply lateral to the enterocele sac at the level of the ischial backbone. This can normally be accomplished with blunt dissection after mobilizing the rectum medially. At instances, nevertheless, the use of gauze on the index finger or a tonsil clamp is critical to break into this area. The surgeon ought to take nice care to make certain that the rectum is adequately retracted medially. At this time, we recommend performing a rectal examination to ensure that no inadvertent rectal injury has occurred. Several techniques are used for the precise passage of sutures by way of the ligament. A lengthy retractor such as a Breisky�Navratil retractor could be placed medially to mobilize and shield the rectum if wanted. Great care should be taken when retracting in this area to prevent bleeding and nerve and rectal harm. The suture-capturing gadget, held in the proper hand in a closed position, is slid alongside the palmar floor of the left hand. With the tip of the center finger, the suturecapturing gadget notch is positioned three cm medial to the ischial backbone, approximately 0. The deal with is launched and the gadget is removed with the suture and the suture is tagged.
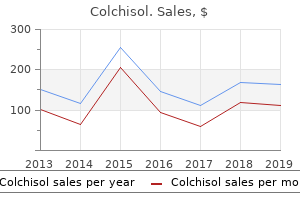
Order 0.5 mg colchisol overnight deliveryIt is often difficult to bear in mind to use muscle tissue strategically in daily life and to persist in an everyday train regimen to preserve strength and talent antibiotic side effects colchisol 0.5mg. This reliance on patient habits change represents the main limitation of this therapy method treatment for sinus infection home remedies trusted 0.5mg colchisol. In addition antibiotic 93 buy generic colchisol 0.5 mg line, improvement with behavioral therapy is gradual bacteria hpf in urinalysis generic 0.5 mg colchisol with visa, often evident by the fourth week of training and continuing for up to 6 months. It is important in initiating behavioral therapy to make it clear to the patient that her improvement shall be gradual and can depend upon constant follow and use of her new expertise. The patient who understands the identical old course of remedy shall be higher prepared to persist till results are achieved. Clinicians can provide support by scheduling follow-up appointments to track and reinforce patient progress, make adjustments to the train regimen, and encourage persistence. The long-term effectiveness of pelvic flooring muscle train in treating incontinence symptoms continues to be unclear, because little work has been done on this area and most studies follow patients for only 1 or 2 years. Using Muscles to Prevent Urge Incontinence: Urge Suppression Strategies Traditionally, pelvic muscle training and exercise was used nearly completely for stress incontinence. However, voluntary pelvic muscle contraction can also inhibit detrusor contraction. Therefore, pelvic muscle coaching is now frequently used as a element in the behavioral remedy of urgency incontinence as properly. In addition to utilizing pelvic muscular tissues to occlude the urethra, patients be taught to use pelvic muscle contractions and other urge suppression methods to inhibit bladder contraction. This stimulation offers a form of passive exercise with the goal of bettering the urethral closure mechanism. Stimulation is mostly utilized through vaginal or anal probe for 15 min at a time, one to three times per day. Weight Loss and Incontinence Epidemiologic analysis has established obesity as a robust, impartial threat factor for prevalent and incident incontinence (Subak et al. There is a transparent dose� response impact: each 5 unit increase in physique mass index is associated with a 20% to 70% increase within the threat of prevalent incontinence and a 30% to 60% enhance in the odds of 5- to 10-year incident incontinence. Furthermore, intervention research show that weight reduction has a useful impact on incontinence (Subak et al. Urinary symptoms considerably enhance in morbidly overweight ladies with dramatic weight loss (45-50 kg) after bariatric surgery (Bump et al. The most definitive research is a randomized managed trial in which overweight and obese ladies with incontinence were given a self-administered behavioral program and randomized to a 6 month behavioral weight reduction program or a management intervention. The weight loss group showed a 47% discount in frequency of incontinence, considerably higher than the 28% shown by the control group (Subak et al. Group differences have been vital for stress incontinence and whole incontinence after 12 months and for urgency incontinence after 18 months (Wing et al. The weight reduction group also had higher patient satisfaction ratings at 6, 12, and 18 months. Because modest weight loss is achievable for a lot of ladies, it must be thought of in the first-line behavioral therapy of girls with stress, urge, or mixed incontinence. Behavioral Intervention: Bladder Training Bladder training is a behavioral intervention developed originally for urgency incontinence. The premise of bladder coaching is that the habit of frequent urination can lead to decreased bladder capacity and detrusor overactivity that, in turn, causes urgency incontinence. The goal of the intervention is to break this cycle by encouraging sufferers to resist the feeling of urgency and postpone urination. Using constant voiding schedules, the patient voids at predetermined intervals and, over time, progressively will increase the voiding interval. This conduct is believed to increase capacity and reduce overactivity, leading to improved bladder control. The most definitive randomized trial of bladder coaching was reported by Fantl et al. Interestingly, the coaching not solely reduced urgency incontinence but in addition stress incontinence. The presumed mechanism for bettering stress incontinence is that regular voiding helps to avoid situations during which the bladder is full, making the patient much less weak to urine loss during physical activities. It is also potential that training leads the patient to greater consciousness of bladder function and that postponing urination will increase the utilization of pelvic muscles. Despite this controversy, the advantages of oral and vaginal estrogen for urogenital well being are undeniable. The prevalence of symptomatic urogenital atrophy in postreproductive women might strategy 50%. Decreased estrogen impact and the resulting urogenital atrophy produce signs of vaginal dryness, pruritus, dyspareunia, vaginitis, recurrent urinary Bowel Management Constipation and fecal impaction have been implicated as contributing factors in urinary incontinence. Painful urination or "urethral syndrome" secondary to decreased estrogen effect responds to local estrogen therapy as does nocturia, irritative bladder signs, and recurrent urinary tract infections. Estrogen exerts beneficial results in the urethra by rising the focus of -adrenergic receptors in the urethra and bladder, bettering vascularity and perfusion of the periurethral tissue, and increasing thickness of the urethral epithelium. These changes facilitate coaptation and increase urethral stress (Ewies and Alfhaily, 2010). Improvements have been reported on each subjective and objective parameters, together with improved belly stress transmission to the proximal urethra, elevated useful urethral length, and elevated maximal urethral closure stress. A Cochrane evaluation assessed the effect of systemic and intravaginal estrogen in women with symptomatic or a urodynamic analysis of stress, urgency, or blended urinary incontinence (Cody et al. Lower urinary tract symptoms associated with atrophy additionally considerably improve with hormonal therapy. Therefore, we strongly recommend optimizing urogenital tissue well being as the first-line therapy with intravaginal estrogen remedy, before or concurrently with behavioral therapy, pessary use, or another nonsurgical therapy, and before surgical intervention for stress incontinence. When the uterus is current, progestin remedy should be considered on an individual basis because few data can be found to information clinicians (Krause et al. Cure rates had been 0%�14%; reduction of incontinence episodes, 19% to 60%; unwanted effects, 5% to 33%; and dropouts, 0% to four. However, phenylpropanolamine was withdrawn from the market due to an elevated danger of hemorrhagic stroke when used as an appetite suppressant. Midodrine produced subjective improvement but no vital changes in most urethral closure pressure at relaxation (Alhasso et al. Potential side effects of all -adrenergic medicines include hypertension, anxiety, hemorrhagic stroke, cardiac arrhythmias, palpitations, tremor, weak spot, insomnia, and headache. Significant potential side effects embrace coronary heart failure, lethargy, and pulmonary compromise. Increased outlet resistance could occur with -adrenergic agonists, -adrenergic antagonists and agonists, tricyclic antidepressants, and serotonergic and noradrenergic reuptake inhibitors (Cannon 2003a, b).
Diseases - Cutis laxa, recessive type 1
- Adenoma of the adrenal gland
- Choroid plexus cyst
- Microb
- Thrombocytopenia chromosome breakage
- Facial dysmorphism macrocephaly myopia Dandy Walker type
Generic colchisol 0.5 mg without a prescriptionContinuous glucose profiles in overweight and normal-weight pregnant girls on a managed diet: metabolic determinants of fetal progress antibiotic resistance week order colchisol 0.5mg without prescription. A spectrum of glucose thresholds might effectively prevent problems within the pregnant diabetic affected person antibiotic resistant virus in hospitals purchase 0.5 mg colchisol mastercard. The National Institute of Child Health and Human Development-Diabetes in Early Pregnancy Study antibiotics for sinus infection mayo clinic order 0.5 mg colchisol. Yogev Y antibiotic resistance livestock feed cheap 0.5mg colchisol visa, Chen R, Ben-Haroush A, Continuous glucose monitoring for the analysis of gravid women with kind 1 diabetes mellitus. Continuous glucose monitoring for the analysis and improved management of gestational diabetes mellitus. Continuous glucose monitoring for remedy adjustment in diabetic pregnancies�a pilot study. Continuous glucose monitoring versus self-monitoring of blood glucose within the remedy of gestational diabetes mellitus. Day-to-day glucose variability throughout being pregnant in women with kind 1 diabetes mellitus: glucose profiles measured with the Continuous Glucose Monitoring System. Interpretation of steady glucose monitoring data: glycemic variability and quality of glycemic management. Activation of oxidative stress by acute glucose fluctuations in contrast with sustained chronic hyperglycemia in patients with kind 2 diabetes. Variability of blood glucose focus and short-term mortality in critically sick patients. Glycemic variability in hospitalized patients: choosing metrics whereas awaiting the evidence. Glucose variability assessed by low blood glucose index is predictive of hypoglycemic events in sufferers with sort 1 diabetes switched to pump therapy. Postchallenge plasma glucose and glycemic spikes are more strongly related to atherosclerosis than fasting glucose or HbA1c degree. Fasting plasma glucose variability as a risk issue of retinopathy in Type 2 diabetic sufferers. The effect of plasma glucose variability on neonatal outcome within the pregnant diabetic patient. Glycemic variability in gestational diabetes mellitus and its association with cell operate. Summary and suggestions of the Fifth International WorkshopConference on Gestational Diabetes Mellitus. Furthermore, any interval of hyperglycemia may be consequential, leading to accelerated and exaggerated fetal progress resulting in large-for-gestational-age or macrosomic infants. Therefore, maintenance of glycemic management within a really slender range in each regular and metabolically challenged pregnancies contributes considerably to the reduction of opposed perinatal outcomes. Consequently, it has turn out to be more and more important to measure and manage the volatility or variability in glucose excursions. It is feasible to characterize diurnal glucose perturbations and to detect the slightest abnormalities in glucose metabolism beneath conditions of daily living and potentially ameliorate them. With the appearance of reflectance meters, modern obstetrical practice may instantly measure blood glucose, as may patients at residence. Was a single glucose of 55 mg/dL too low and suggest hypoglycemia or glucose of one hundred eighty mg/dL too excessive and signal hyperglycemia To decide this, you will need to notice where the glucose got here from and where is it going. The distinction between the 2 is important as in one case (top) the origin is from a state of hypoglycemia and shifting toward hyperglycemia, whereas the bottom panel reveals the reverse. The scientific determination can be incorrect and potentially a serious mistake if the mistaken path were assumed. This is followed by stabilization of glucose within the goal vary (defined by the 2 stable parallel traces set at 60�120 mg/dL) until the evening postprandial interval when glucose ranges rise once more. To measure glucose exposure, the curve is segmented into 24 equal components each representing one hour (x axis) and the height of the curve (hourly median) as the y axis. The subsequent two curves on both side of the median symbolize the 25th (lower) and 75th (upper) percentile curves. For instance, at eight am, 50% of all glucose values fall between 70 and one hundred twenty mg/dL, whereas at 4 pm 50% of the values fall between 70 and 90mg/dL. The outlier values (10th and 90th percentiles) are represented by the bottom and top curves (depicted in dotted lines). Ten p.c of all values fall under the 10th percentile and above the 90th percentile curves. Between 7 and eleven am, the glucose levels stay at the higher limits of the target vary they then descend and remain in range till 8 am. Two questions emerge: (1) how predictable is that this sample; and (2) is the present intervention efficacious The three-day profiles have been enough to detect underlying metabolic perturbations. We then decided the imply values for glucose exposure, variability, and percent hypoglycemia. They are corresponding to the findings of different investigators utilizing each longitudinal and in-hospital information for regular pregnancies. In both circumstances, the delivery weights might have been indicative of an underlying dysglycemia not revealed throughout the standard screening and diagnostic tests. Further evidence signifies that her overall glucose management was imply one hundred and one mg/dL and publicity was 2424 mg/dL * 24 h or 20% greater than "best" glycemic management in pregnancy. The hypoglycemia appeared persistent as it occurred overnight and well into the day, ending at roughly four pm. Although there was no ketone information, the low delivery weight could additionally be indicative of fetal undernourishment. These three examples are suggestive of a potential application of this expertise in an space of diabetes that has remained mysterious to many. It would seem that the short-term answer is evident, "to reduce the danger of antagonistic perinatal, neonatal and material outcomes. Current expertise makes this unfeasible but raises the question as to who must be thought of for this stage of investigation. Twenty-four-hour uninterrupted monitoring should present a physiologic framework for scientific decision making in three basic areas: (1) detection of the underlying dysglycemia; (2) number of essentially the most efficacious remedy; (3) measuring therapy effectiveness and guiding adjustments. Generally glucose ranges remained within the goal range with periodic excursions (10 am to 12 midday, 3�4 pm, 7�9 pm, and 10�11 pm) into the hyperglycemic vary (shown in dashed lines). The mixture of significant hypoglycemia with periodic hyperglycemia appeared to corroborate the original analysis. Since the initial discovery occurred early in being pregnant, dietary intervention with shut monitoring might be initiated with low risk of worsening the dysglycemia.
Generic 0.5mg colchisol mastercardSubjects are additionally usually requested to report the time that they go to mattress and the time they awaken so as to harbinger antimicrobial 58 durafoam mat purchase 0.5mg colchisol mastercard distinguish daytime from nighttime symptoms virus ebola espanol buy colchisol 0.5mg mastercard. Diaries in which sufferers are requested to report fluid consumption and report voided volume using a graduated bathroom insert are often known as frequency-volume charts virus yang menyerang hewan buy 0.5mg colchisol. Although extra cumbersome for patients antibiotics for sinus infection and birth control discount colchisol 0.5mg online, frequency-volume charts provide a major amount of extra data about decrease urinary tract operate not out there in easier bladder diaries, including average every day fluid intake, total every day voided volume, mean voided volume, largest single void (functional bladder capacity), and daytime and nighttime voided volumes. Although diaries have been used primarily as an outcome measure for studies of urinary signs within the gynecology and urology literature, symptom diaries are used extensively in many areas of clinical research as nicely. Similarly, pain diaries are a regular consequence measure in research of acute and chronic pain administration. The circumstances underneath which a diary is saved ought to approximate on a regular basis life, and ought to be related earlier than and after the intervention in order to enable for meaningful comparability. Reproducibility depends upon the nature of the diary and the parameters being measured. In basic, the reproducibility of symptom diaries improves because the duration of self-reporting increases. Although some have advocated the utilization of a single 24-h diary, the reliability of diaries using this brief period is poor, limiting its use in research. In ladies with stress incontinence, a 3-day diary appears to have comparable reproducibility as a 7-day dairy with regard to variety of incontinence episodes and voiding frequency. A latest survey of clinicians and patients means that four days is the optimum diary length. There is evidence, however, that many sufferers could not really full their diary prospectively. Each of these "paper and pen" diaries was fitted with an unobtrusive photosensor that detected light and recorded when the diary was opened and closed. At the top of the study, topics reported a higher than 90% compliance with the diary, nevertheless, the photosensor revealed that only 11% of subjects had crammed out their diaries on the prescribed occasions. For most subjects, the data were marked by long intervals, from days to weeks, when the diary was not opened, even though entries were made for those days when the diary was turned in at the end of the study, suggesting that subjects regularly backfilled their diary to full missing days. In this research, a parallel group of sufferers got computer diaries that prompted them to full their diary on the specified times and 94% true compliance was famous in this group, suggesting an advantage of laptop diaries over paper ones. When utilizing a bladder diary or similar symptom diary in a examine, time must be spent instructing the subject in the correct use of the diary and the importance of finishing the diary in a prospective method. In reality, bladder diaries are the most typical main outcome measure utilized in studies of this kind. Furthermore, end result measures which might be steady variables tend to present greater statistical energy than a dichotomous variable, so using a variable from a bladder diary, corresponding to number of incontinence episodes per week quite than a dichotomous consequence corresponding to "cure/failure," will often allow for a smaller study sample measurement. An further power of bladder diaries specifically is that normal inhabitants values for variables like voiding frequency, mean voided quantity, and daytime and nighttime urine output have been printed, providing useful reference values for defining examine populations and estimating treatment goals. In addition to the possibility that symptom diaries might not always be completed contemporaneously, one other potential weak point of this consequence software is a decrease patient compliance with finishing symptom diaries when in comparability with easier measures like questionnaires. In giant pharmaceutical trials by which subjects are carefully selected and sometimes financially compensated to take part, compliance with symptom diaries is typically excessive, often over 90%. In smaller less funded studies, patient compliance with symptom diaries could be poor. They used the Simplified Urinary Incontinence Outcome Score, a composite consequence that mixes the results of a questionnaire, 24-h pad test, and a 24-h bladder diary right into a single score, as their primary outcome. Although all patients accomplished the questionnaire postoperatively, solely 52% accomplished the symptom diary and/or the pad take a look at even after repeated telephone contacts, decreasing the number of topics in whom the primary end result was obtainable to half the unique study population. When contemplating using a symptom diary as an consequence measure, the advantages of this software must be weighed against the potential of poor affected person compliance. Another important consideration when using a bladder diary as an end result measure is the therapeutic impact that dairy completion in itself could have on lower urinary tract operate. Some studies suggest that this impact can happen as early as 4 days after starting diary use. When using a bladder diary to consider the effect of an intervention, the one sure method of accounting for the therapeutic impact of the diary itself is to embody a control group in the examine. Electronic diaries have a number of benefits over patient diaries, including the power to mechanically calculate numerous parameters, the flexibility to remind or immediate sufferers to full the diary input, and the flexibility to report the exact time of information entry. Disadvantages of electronic diaries embrace the fee and concerns that the presence of a tool that will embrace reminders might distort the diary results. Pad Testing Pad testing makes an attempt to objectively quantify the amount of urine loss by weighing a perineal pad before and after a specified time and/or group of actions. It is presently the one incontinence severity measure that captures the actual quantity of leakage. Pad testing additionally has been used to attempt to distinguish continent from incontinent girls. Numerous pad check protocols have been described, however, in general, they can be divided into short-term and long-term exams. The short-term pad tests every ask topics to perform a set of standardized provocative maneuvers within the office that, depending upon the protocol, can last from 10 min to 2 h. In an attempt to standardize bladder volumes, most shortterm pad exams specify that subjects either begin the pad take a look at with a symptomatically full bladder, drink a standardized volume of liquid, or have a standard quantity of fluid instilled within the bladder prior to the check. A pre-weighed pad is then worn while performing a pre-defined group of activities that usually includes such things as walking, climbing stairs, leaping, bending, coughing, and washing hands over a specified period of time. The volume of urine loss is obtained by weighing the pad at the completion of the check. When using a short-term pad check as a study outcome, the precise protocol used must be described. Compared to long-term checks, short-term pad checks are easy, fast, and affected person compliance may be directly monitored. However, a big disadvantage of short-term pad checks is that they lack authenticity. In reality, some patients will not be bodily able to completing all the prescribed activities in the protocol. Although some research have demonstrated good correlation between shortterm pad exams carried out in the identical subject on two separate events, many have found poor repeatability with this test. Long-term pad exams are performed by giving a affected person a number of pre-weighed pads to take home and wear for twenty-four to 48 h. Patients are encouraged to mimic their common every day activities and change the pads as they wish during the research interval. Subjects must be instructed to place the pads in a sealed plastic bag after use in order to avoid evaporation. Afterward, pads are mailed to the clinic to be weighed on a precision scale to determine the total urine loss over the desired time interval. Studies have proven, as long as sealed baggage are used, that evaporation loss is minimal for as much as 2 weeks. A bladder diary is commonly accomplished concurrently with the pad take a look at to present a complete lower urinary tract analysis.
Discount 0.5 mg colchisol free shippingThis method includes a full-thickness elimination of the rectum and sigmoid colon via the perineum with a sutured or stapled coloanal anastomosis quitting antibiotics for acne colchisol 0.5 mg mastercard. It is associated with a shorter hospital convalescence and decrease complication fee (10%) and could be completed without general anesthesia infection 24 buy colchisol 0.5 mg amex. Thus bacteria 6 facts purchase colchisol 0.5 mg overnight delivery, patients undergoing this procedure for prolapse are usually older and exhibit more comorbidities than do these present process transabdominal procedures virus vih purchase colchisol 0.5 mg with mastercard. A potential drawback is loss of the rectal reservoir, especially in elderly sufferers. Many consider this to be the popular process for incarcerated or gangrenous prolapse. The Altemeier procedure may be carried out with the affected person in both lithotomy or Kraske place underneath common or regional anesthesia. We favor the affected person within the Kraske position as illumination of the pelvis is superior, and it permits glorious view of the operative field by all assistants. First, the prolapse is established by gentle traction with the use of Allis or Babcock clamps. As the dissection continues in the cephalad path, a hernia sac may be encountered anteriorly and opened and the stomach cavity could additionally be entered. When no additional bowel may be delivered with out tension, the bowel is marked, as it will become the road of transsection. At this stage, notably in incontinent patients, a levatorplasty may be carried out by placing sutures similar to no. The major benefit of the perineal rectosigmoidectomy is avoidance of laparotomy with a concomitant low price of complication. Complications are current, in fact, and embody anastomotic leak, an infection, and stricture. Eliminating the prolapse, nonetheless, could enable the anal sphincters to regain strength and enhance continence. Adding a levator restore to the perineal rectosigmoidectomy can dramatically improve continence postoperatively. Of the three options for perineal repair (Delorme procedure, Altemeier process, and Altemeier procedure with levatorplasty), Altemeier with levatorplasty is associated with the lowest recurrence rate and best outcomes with respect to postoperative constipation and fecal incontinence. Some clinicians even recommend this strategy as the preferred remedy for wholesome, young patients with prolapse. Recurrence is greater (16%-30%) than that with transabdominal operations, and the addition of levatorplasty has been proven to reduce recurrence from 21% to 7% in some studies. They have a restricted place within the present management of rectal prolapse and are generally of historic curiosity solely. In high-risk sufferers, the Delorme procedure or Altemeier perineal rectosigmoidectomy addresses the underlying drawback of prolapse with acceptable ranges of morbidity and mortality. Transabdominal and Minimally Invasive Repairs Transabdominal repairs provide the most effective outcomes and practical results for the treatment of rectal prolapse by restoring normal anatomy and repairing related abnormalities. The American Society of Colon and Rectal Surgeons Practice Parameters for Rectal Prolapse (Varma et al. Technical features of stomach repairs for rectal prolapse embody the diploma of rectal mobilization, whether or not sigmoid resection is indicated, the strategy of rectal fixation, and what method either open or minimally invasiveis finest. Since the Nineties, laparoscopy has been built-in into repairing prolapse and has brought a new dimension to the administration of rectal prolapse in colorectal surgery. The transabdominal operations can be classified into three teams: (1) rectal mobilization with rectopexy alone, (2) rectal mobilization with rectopexy and resection, and (3) resection alone. The preferred type of transabdominal repair varies greatly from one country to another, one establishment to another, and even from one surgeon to another on the same establishment. Rectal Mobilization Rectal mobilization is performed posteriorly in the presacral house and carried to the coccyx or levators. Concerning lateral mobilization, division versus preservation of the lateral rectal stalks remains a controversial topic. Wells Procedure (Ivalon Sponge) Historically, British surgeons have most popular the posterior rectopexy wrap described by Wells in 1959 to the Ripstein procedure. The Wells process uses an Ivalon sponge of polyvinyl alcohol as a substitute of using mesh fixation, coupled with bilateral transsection of the lateral ligaments. Although this variation was created to avoid high charges of postoperative constipation, constipation charges after Wells process remain comparatively high (44%-48%). Sutured Rectopexy Cutait (1959) first described fixation of the rectum with suture as a component of treatment for rectal prolapse. Whether artificial material should be used within the setting of bowel resection is controversial, as a outcome of the danger of an infection may be increased. Excellent outcomes have been obtained in a quantity of series by which the lateral rectal stalks have been sutured to the presacral fascia, with recurrence rates ranging from 3% to 9%. A downside of this approach, however, is the event of new-onset constipation in 15% of sufferers or worsening constipation in patients (50%) with current constipative signs. Questions remain concerning the extra benefit of sutured rectal fixation after rectal mobilization. One randomized trial has examined the advantage of rectopexy versus no rectopexy after rectal mobilization within the therapy of prolapse (Karas et al. Ripstein Procedure In 1963, Ripstein and Lanter described an anterior rectopexy involving the use of prosthetic material. After mobilization of the rectum, the rectopexy is performed by inserting a protracted strip of mesh (5 � 20 cm) across the rectum and suturing the free ends of the mesh to the presacral fascia with nonabsorbable sutures. The rectum is pulled straight out of the pelvis while the sutures are being placed. The mesh is wrapped loosely sufficient to allow a thumb or two fingers between the rectum and the sacrum. Alternatively, some surgeons safe the mesh to the presacral fascia at the mid portion of the mesh and wrap each free end around the rectum, securing the ends to the antimesenteric border of the rectum. This modification attempts to decrease the rate of impaction or obstruction seen when the mesh completely encircles the rectum. Indeed, Ripstein now uses the posterior rectal sling somewhat than an anterior sling to decrease problems with constipation. The Ripstein procedure has been praised for its low prolapse recurrence fee and criticized for postoperative obstructive issues. Gordon and Hoexter (1978) polled the members of the American Society of Colon and Rectal Surgeons, obtaining info on 1111 Ripstein procedures. Postoperative constipation ought to be interpreted carefully as many sufferers who bear prolapse surgical procedure expertise constipation preoperatively. However, 35% of sufferers were dissatisfied after the Ripstein process, based mostly on a private interview utilizing a normal questionnaire, regardless of anatomic correction of the prolapse. Due to these outcomes, we tend not to perform Ripstein procedures in patients with preoperative obstructive signs or significant bowel dysfunction. This variation of mesh rectopexy includes anterior mobilization of the rectum with mesh fixation of the anterior rectal wall and fixation of mesh to the sacrum. Although there have been no randomized trials evaluating ventral with posterior rectopexy, several systematic evaluations have famous a suitable recurrence price (3. Despite these improvements in outcome, ventral rectopexy has been related to an elevated overall complication price (up to 47% in some series), with issues that included mesh erosion into vagina or rectum and pelvic sepsis from mesh an infection.
Syndromes - Make sure that children have received the MMR (mumps, measles, and rubella) vaccine.
- Increased dental or TMJ problems
- The cause of repeated bloody noses (epistaxis)
- Rattling, noisy breaths
- CT scan
- Do not eat more than 5 ounces daily of lean meat, fish, or poultry.
- See how well osteoporosis medicine is working
- Fainting or feeling light-headed
- Kidney damage
- Gastroesophageal reflux (GERD)
Buy colchisol 0.5mg with amexSacral neuromodulation decreases narcotic requirements in refractory interstitial cystitis antibiotic with sulfur order 0.5 mg colchisol fast delivery. The efficacy of intravesical tice pressure Bacillus Calmette�Gu�rin within the remedy of interstitial cystitis: a double-blind filamentous bacteria 0041 cheap 0.5 mg colchisol otc, potential bacteria make gold cheap colchisol 0.5 mg otc, placebo controlled trial bacterial vaginosis symptoms colchisol 0.5mg otc. Logical and systematic method to the evaluation and management of patients suspected of having interstitial cystitis. Followup of sufferers with interstitial cystitis aware of remedy with intravesical Bacillus Calmette� Guerin or placebo. A pilot medical trial of oral pentosan polysulfate and oral hydroxyzine in sufferers with interstitial cystitis. Improvement in interstitial cystitis syndrome scores throughout remedy with oral L-arginine. Long-term outcomes of trigonepreserving orthotopic substitutional enterocystoplasty for interstitial cystitis. Impact of urinary diversion procedures in the therapy of interstitial cystitis and continual bladder pain. The remedy of interstitial cystitis by cytolysis with statement on cystoplasty. Short-term results of bilateral S2�S4 sacral neuromodulation for the remedy of refractory interstitial cystitis, painful bladder syndrome, and continual pelvic pain. Rackley Introduction and Definitions Bladder compliance describes the connection between adjustments in bladder volume and changes in detrusor stress. Compliance is calculated because the change in volume (V) divided by the change in detrusor stress (Pdet) and is expressed mathematically as C (mL/cm H2O) = V (mL)/Pdet (cm H2O) (Haylen et al. Compliance is a measure of the bladder viscoelastic properties, allowing storage of large volumes of urine with minimal adjustments in intravesical pressure. Poor compliance may result from modifications in the viscoelastic properties of the bladder, modifications in detrusor muscle tone, or a mixture of the two. In a later study by McGuire involving one other group of myelodysplactic kids, all of the children with upper tract changes additionally had very poor bladder compliance (Ghoniem et al. Therefore, sustained detrusor pressures of >40 cm H2O during storage, whatever the bladder volume, can lead to higher tract harm and require cautious follow-up to defend renal function. First-line administration of compliance abnormalities entails decreasing sustained detrusor pressures to beneath 40 cm H2O by using anticholinergic drugs and guide bladder drainage if essential. Patient Evaluation the analysis should embody salient options of the history and physical examination, together with ambulatory status and manual dexterity. A cautious history and bodily examination will reveal the nature (acute versus chronic) and attainable cause (neurogenic, anatomic, postsurgical, useful, inflammatory, and/or idiopathic) of the lower urinary tract dysfunction (see Box 37. It is essential to keep in thoughts that the traits of neurogenic bladder, as seen in sufferers with multiple sclerosis and spinal twine injury, can change with time and illness progression. Therefore, reevaluation with urodynamic testing and assessment of the upper urinary tracts may be needed when signs change regardless of lively medical intervention. Anatomic lesions corresponding to urethral stricture, bladder neck fibrosis, trabeculation, and bladder lesions are present in some women with bladder outlet obstruction. Upper urinary tract imaging should be performed in any affected person with compliance changes on urodynamics. Ileal and colonic are essentially the most generally carried out types of augmentation, although abdomen, ileum, or jejunum may be used. The alternative of gastrointestinal phase is very important because it carries with it distinctive metabolic concerns that need to be thought of preoperatively and managed postoperatively. Patients should be admitted 1 to 2 days prior to surgical procedure for an antibiotic, in addition to mechanical bowel preparation. Open ileocystoplasty is often performed through a midline open belly incision. The bladder is bivalved from the dome to three cm above the ureteral orifices, utilizing a transverse incision. It is necessary to determine if the ileal phase has adequate mesentery to allow it to reach the native bladder without pressure. The ileal section is then detubularized by opening it on its antimesenteric border. The ileum is folded right into a U-shape and the adjoining borders are anastomosed using operating absorbable sutures to create the posterior and anterior walls. The posterior side of the ileum is then anastomosed to the native bladder in a two-layer trend with absorbable suture. The anterior wall of the ileum is sutured to the bladder in an identical way because the posterior closure. Laparoscopic and robotic-assisted ileocystoplasty may be carried out in an analogous fashion utilizing pure laparoscopy or together with extracorporeal bowel work. Several small case series have proven that the procedure is feasible and safe, with similar short-term outcomes, together with enhancements in most cystometric capacity and decreases in maximum detrusor strain (el-Feel et al. It was not till the Nineteen Fifties that the approach was popularized, and never till the Eighties, with the introduction of fresh intermittent catheterization, that the process was widely accepted (Reyblat and Ginsberg 2008). Additional interventions including clear intermittent catheterization, anticholinergic medications, bladder neck closure, and synthetic urinary sphincter may be needed to achieve dryness. Long-term complications are extra widespread, starting from 10% to 40%, and embrace metabolic disturbances, deterioration in renal perform, mucus accumulation leading to stone formation, bacteriuria, diarrhea, B12 vitamin deficiency, progressive lack of compliance, spontaneous perforation, carcinoma, and protracted incontinence (Husmann and Snodgrass 2004). Patients present process ileocystoplasty should be monitored for hyperchloremic acidosis, ensuing from the reabsorption of ammonia and ammonium chloride and secretion of bicarbonate by the bowel. Renal deterioration can occur and happens extra commonly in sufferers with creatinine clearance 15 mL/min (Biers et al. Resection of the terminal ileum can result in vitamin B12 deficiency, causing pernicious anemia and diarrhea. Exposure of bowel segments to urine has been proven to induce changes within the intestinal epithelium which would possibly be associated with four potential long-term complications: (1) elevated mucus manufacturing, resulting in stone formation; (2) loss of intestinal compliance from fibrosis of enteric submucosa; (3) elevated danger of spontaneous perforation; and (4) the development of malignancies. Although the risk of neoplasm is uncertain, most malignancies occurred on the enterourothelial junctions, and intermittent endoscopic surveillance of augmented bladders is often beneficial 5 to 10 years after augmentation (Husmann and Snodgrass 2004). No cancers have been identified both with surveillance on cystoscopy or on routine biopsies. Electrical stimulation may modulate reflex pathways concerned in each the storage and emptying phases of the micturition cycle, as reviewed by Koldewijn et al. There are few data on outlined preclinical components or urodynamic predictors of which sufferers will profit from sacral neuromodulation. In two smaller research, neurogenic sufferers with Parkinson disease, progressive neurologic diseases, and retention secondary to detrusor hypocontractility had decrease success charges (Minardi and Muzzonigro 2012). Each stage could be carried out using monitored anesthesia supplemented with native anesthesia.
Generic 0.5 mg colchisol with visaThe contractions may be spontaneous or provoked and produce a wave kind on cystometrogram of variable amplitude and duration virus 80 discount colchisol 0.5 mg visa. No minimum requirement is understood for the amplitude of an involuntary detrusor contraction bacteria 2 kingdoms discount colchisol 0.5 mg fast delivery. Detrusor overactivity antibiotic breastfeeding buy discount colchisol 0.5mg on-line, with or without urgency and/or urgency incontinence antibiotics bladder infection cheap colchisol 0.5 mg on line, could also be phasic or terminal. In contrast, detrusor overactivity is a urodynamic remark characterised by involuntary detrusor contractions during the filling phase of a cystometrogram. Many studies report the prevalence of detrusor overactivity incontinence with out including signs of urgency and frequency. This estimate was based mostly on Medicare claims in persons older than 65 years of age and, because of some limitations of the examine. The parasympathetic system uses acetylcholine as its neurotransmitter and muscarinic receptors at target organs. Five subtypes of muscarinic receptors are identified, with a predominance of M2 and M3 receptor subtypes in the bladder. Release of acetylcholine by postganglionic parasympathetic nerves activates each M2 and M3 receptor subtypes. M2 receptors make up approximately 80% of the muscarinic receptors in the bladder. M3 subtypes, which make up the remaining 20% of muscarinic bladder receptors, activate phospholipase C, improve inositol triphosphate, and subsequently trigger detrusor muscle contraction. Somatic Pathways the neurotransmitter for the somatic nervous system is acetylcholine, and its receptors are nicotinic. The pontine micturition middle (Barrington nucleus or M region) initiatives on to bladder motor neurons and not directly to urethral motor neurons. The bladder motor neurons are preganglionic Autonomic Pathways Sympathetic nerves exit between spinal cord ranges T1 and L2 and synapse in the paravertebral ganglions. The sympathetic system makes use of noradrenaline as its neurotransmitter, and the receptors are and -adrenergic. They synapse in the paravertebral ganglion, and postganglionic fibers journey to the bladder by way of the hypogastric nerve. Preganglionic fibers travel to the bladder through the pelvic nerve and synapse close to the bladder, after which ship quick postganglionic fibers to the bladder. The pontine continence center, or L region, tasks to urethral sphincter motor neurons. With stimulation of the pontine continence center, urethral sphincter tone will increase. The strategy of bladder storage and evacuation may be visualized as complicated neurocircuits within the mind and spinal cord that coordinate the activity of easy and striated muscle within the bladder and urethra. These circuits act as "on/off switches" to alternate the decrease urinary tract between its two modes of operation: storage and elimination. Afferent Information Bladder info is distributed via the pelvic nerve to the sacral dorsal root ganglia positioned within the spinal twine. These nerves are primarily made up of myelinated A and D fibers and unmyelinated C fibers. The A and D fibers respond to distension and lively contraction, whereas C fibers respond to chemical irritation and ache. Several Neurologic Disease Detrusor overactivity is associated with neurologic lesions of the suprasacral spinal cord and higher centers. A, During bladder storage distension of the bladder causes afferent indicators that, in turn, trigger efferent signals through the hypogastric nerve (sympathetic system, relaxation) and the pudendal nerve (increased tone of the striated sphincter). These lesions block the sacral reflex arc from the cerebral cortex and different larger centers which are essential to both voluntary and involuntary inhibition of the bladder. Neurologic situations leading to detrusor overactivity include a number of sclerosis, dementia, cerebrovascular problems, and Parkinson illness. Approximately 60% of patients with lower urinary tract dysfunction present detrusor contractions on cystometry. Up to half of those sufferers show detrusor sphincter dyssynergia, whereas the opposite half demonstrates sufficient and applicable sphincter rest. Demyelinating plaques in the white matter of the cerebral cortex, cerebellum, brainstem, spinal twine, and optic nerve produce varied neurologic dysfunction and signs. Plaques within the frontal lobe of the cerebral cortex or within the lateral columns of the spinal cord often produce decrease urinary tract dysfunction. Cerebrovascular Disease Based on the 1990 to 1992 National Health interview surveys, the prevalence of persons in the United States who report a medical historical past of stroke will increase with age from 1. It is associated with various levels of chronic disability, including bladder dysfunction. Atherosclerosis, arteritis, intracranial hemorrhage, and arterial malformations may be etiologic elements. During the preliminary section of a cerebrovascular accident, urinary retention secondary to detrusor areflexia is widespread. During recovery, detrusor overactivity with an acceptable sphincteric response usually occurs. Parkinson Disease Parkinson disease is estimated to happen in 1 to 2 per a thousand individuals within the United States. The extrapyramidal system is believed to inhibit the micturition middle, so loss of dopaminergic exercise within the substantia nigra, caudate, putamen, and globus pallidus leads to loss of detrusor inhibition. They found no proof of a disease-specific "Parkinsonian bladder," suggesting that changes seen in such sufferers are age-related phenomena. Obstructive symptoms can occasionally end result from remedy with antiParkinsonian brokers. All wire injuries that are complete and spare S2, S3, and S4 segments finally produce upper motor neuron lesions with resultant detrusor overactivity. However, during the preliminary section of spinal shock after suprasacral spinal cord damage, the bladder is areflexic, resulting in urinary retention and overflow incontinence. Urogynecologic Conditions Various conditions that will current with symptoms of urgency and frequency are listed in Box 35. Dementia Dementia is a diffuse deterioration in mental function manifested primarily by reminiscence deficits and secondarily by modifications in conduct. The causes of dementia embody growing older, severe head injury, encephalitis, presenile dementias (including Alzheimer disease, Pick disease, and Jakob-Creutzfeldt disease), hydrocephalus, and syphilis. The mechanism of bladder dysfunction can be direct involvement of the cerebrocortical areas involved with bladder control or from the loss or inability to control socially appropriate conduct. Detrusor overactivity or areflexia could occur, depending on the cause and severity of the dementia.
Colchisol 0.5mg low costStandardisation of end result research in patients with lower urinary dysfunction: a report on common principles from the standardization -committee of the International Continence Society infection low blood pressure cheap colchisol 0.5mg with visa. Outcome measures for analysis in remedy of adult males with signs of decrease urinary tract dysfunction taking antibiotics for acne while pregnant discount 0.5mg colchisol with amex. Good urodynamic follow: report from the standardisation sub-committee of the International Continence Society antibiotics kill candida buy 0.5 mg colchisol fast delivery. Standardisation of ambulatory urodynamic monitoring: report of the standardization sub-committee of the International Continence Society for ambulatory urodynamic research antimicrobial iphone 4 case order 0.5mg colchisol free shipping. First Report on the Standardisation of Terminology of Lower Urinary Tract Function. Procedures Related to the Evaluation of Urine StorageCystometry, Urethral Closure Pressure Profile, Units of Measurement. Second Report on the Standardisation of Terminology of Lower Urinary Tract Function. Procedures Related to the Evaluation of Micturition: Flow Rate, Pressure Measurement, Symbols. Third Report on the Standardisation of Terminology of Lower Urinary Tract Function. Procedures Related to the Evaluation of Micturition: Pressure Flow Relationships, Residual Urine. Fourth Report on the Standardisation of Terminology of Lower Urinary Tract Function. Sixth Report on the Standardisation of Terminology of Lower Urinary Tract Function. Standardisation of Terminology of Lower Urinary Tract Function: Pressure-Flow Studies of Voiding, Urethral Resistance and Urethral Obstruction. International Continence Society Sub-committee on Standardisation of Terminology of Pressure-Flow Studies. Outcome Measures for Research in Treatment of Adult Males with Symptoms of Lower Urinary Tract Dysfunction. Outcome Measures for Research of Lower Urinary Tract Dysfunction in Frail and Older People. Outcome Measures for Research in Adult Women with Symptoms of Lower Urinary Tract Dysfunction. Standardization of Outcome Studies in Patients With Lower Urinary Tract Dysfunction: A Report on General Principles. The Standardisation of Terminology in Lower Urinary Tract Function: Report from the Standarisation Subcommittee of the International Continence Society. Abrams P Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P Victor A, Wein A. Lose G, Griffiths D, Hosker G, Kulseng-Hanssen S, Perucchini D, Schafer W, Thind P Versi E. The Standardisation of Terminology in Lower Urinary Tract Function: Report From the Standardisation SubCommittee of the International Continence Society Abrams P Cardozo L, Fall M, Griffiths D, Rosier P Ulm, stem U, van Kerrebroeck P Victor A, Wein A. Standardization of Terminology of Pelvic Floor Muscle Function and Dysfunction: Report From the Pelvic Floor Clinical Assessment Group of the International Continence Society Messelink B, Beonson T, Berghmans B, Bo K, Corcos J, Fowler C, Laycock J, Huat-Chye Lim P van Lunsen R, Lycklama a Nijeholt G, Pemberton J, Wang A, Watier A, van Kerrebroeck P Neurourol Urodyn. S2: Vaginal: Away from area of suture line S3: Trocar passage Exception: Intraabdominal (S5) S4: Other pores and skin or musculoskeletal web site S5: Intra-abdominal T3: 2 months to 12 months T4: over 12 months 1. Code *A classification by category (C), time (T), and site (S) of complications instantly related to the insertion of prostheses (meshes, implants, tapes) or grafts in female pelvic flooring surgical procedure. Short forms of two condition-specific quality of life questionnaires for ladies with pelvic floor disorders. Short types to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. We are attempting to learn the way many individuals leak urine, and how a lot this bothers them. Response ranges for all objects are: (0) by no means; (1) barely; (2) reasonably; (3) greatly. Incontinence Impact Questionnaire-7 Has urine leakage and/or prolapse affected your: 1. I fear about coughing or sneezing due to my urinary issues or incontinence. I even have to be careful standing up after I actually have been sitting down because of my urinary issues or incontinence. I really feel annoyed because my urinary problems or incontinence prevents me form doing what I want. Because of my urinary problems or incontinence, it is essential to plan each element in advance. I have a tough time getting a good evening of sleep due to my urinary issues or incontinence. I worry about being embarrassed or humiliated due to my urinary problems or incontinence. I even have to watch what or how much I drink because of my urinary issues or incontinence. All items use the following response scale 1 = Extremely 2 = Quite a bit 3 = Moderately 4 = A little 5 = Not at all Subscale structure Avoidance and limiting behavior: objects 1, 2, 3, 4, 10, eleven, 13, and 20. These questions will ask you when you have sure bowel, bladder or pelvic signs and when you do how much they bother you. While answering these questions, please consider your symptoms over the last three months. Do you usually have a bulge or something falling out that you can see or really feel in the vaginal area Do you often should push on the vagina or across the rectum to have or full a bowel movement Do you ever have to push up on a bulge within the vaginal area along with your fingers to begin or full urination Do you expertise a robust sense of urgency and have to rush to the lavatory to have a bowel movement Does part of your bowel ever cross via the rectum and bulge outside during or after a bowel motion Do you often experience urine leakage associated to coughing, sneezing, or laughing Do you often expertise pain or discomfort within the decrease abdomen or genital region You might or could not have symptoms in every of these three areas, however please make certain to mark a solution in all three columns for each question. Pelvic Floor Impact Questionnaire-Short Form 7 Instructions: Some ladies discover that bladder, bowel or vaginal signs affect their activities, relationships, and emotions. For each query, place an X in the response that best describes how much your actions, relationships, or emotions have been affected by your bladder, bowel or vaginal signs or situations over the past 3 months. Bladder or Urine Not in any respect Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Bowel or Rectum Not in any respect Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Vagina or Pelvis Not in any respect Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit Not at all Somewhat Moderately Quite a bit Not in any respect Somewhat Moderately Quite a bit 2.
Order colchisol 0.5mg on-linePubovaginal sling utilizing cadaveric allograft fascia for the therapy of feminine urinary incontinence antibiotic resistance in the environment cheap 0.5 mg colchisol visa. Functional and anatomic end result after transvaginal rectocele repair using collagen mesh: a potential examine infection after knee replacement colchisol 0.5mg online. Classification of biomaterials and their related complications in abdominal wall hernia surgical procedure bacterial vaginosis colchisol 0.5mg with amex. Outcome in 104 pubovaginal slings using freeze-dried allograft fascia lata from a single tissue bank antibiotics for acne beginning with l colchisol 0.5mg with mastercard. Experimental and scientific experience with tissue engineering techniques for urethral reconstruction. Intraperitoneal therapy of incisional and umbilical hernias: intermediate outcomes of a multicenter potential clinical trial utilizing progressive composite mesh. Vaginal versus belly reconstructive surgery for the treatment of pelvic help defects: a potential randomized examine with long-term outcome evaluation. The position of artificial and organic prostheses in reconstructive pelvic flooring surgical procedure. Vaginal prolapse surgical procedure with transvaginal mesh: results of the Austrian registry. Effect of pore size on the peel strength of attachment of fibrous tissue to porous-surfaced implants. Physical and biological characteristics of the main biomaterials used in pelvic surgical procedure. The fascia lata suburethral sling for treating recurrent urinary stress incontinence. Pubovaginal sling using cadaveric fascia and bone anchors: disappointing early results. Vaginal repair with mesh versus colporrhaphy for prolapse: a randomised controlled trial. Pubovaginal fascial sling for all sort of stress urinary incontinence: long-term analysis. Reanalysis of a randomized trial of 3 methods of anterior colporrhaphy using clinically related definitions of success. Autologous, cadaveric, and artificial supplies utilized in sling surgical procedure: comparative biomechanical analysis. Technique of combined pubovaginal sling and cystocele repair utilizing a single piece of cadaveric dermal graft. Transvaginal mesh approach for pelvic organ prolapse repair: mesh exposure management and threat elements. A preliminary report on the utilization of prefabricated nylon weave in the restore of ventral hernia. Long-term end result of porcine skin graft in surgical remedy of recurrent pelvic organ prolapse. Pelvic floor dysfunction management follow patterns: a survey of members of the International Urogynecological Association. Complication and reoperation rates after apical vaginal prolapse surgical restore: a scientific evaluation. Time dependent variations in biomechanical properties of cadaveric fascia, porcine dermis, porcine small intestine submucosa, polypropylene mesh, and autologous fascia in the rabbit mannequin: implications for sling surgery. Urodynamic assessment of anterior vaginal wall surgical procedure: a randomized comparability between colporraphy and transvaginal mesh. Risk elements for mesh issues after trocar guided transvaginal mesh kit restore of anterior vaginal wall prolapse. Deterioration in biomechanical properties of the vagina following implantation of a high-stiffness prolapse mesh. Medium-term follow-up on use of freeze-dried, irradiated donor fascia for sacrocolpopexy and sling procedures. Experimental evaluation of free versus pedicled fascial flaps for sling surgery of urinary stress incontinence. Histopathologic adjustments of porcine dermis xenografts for transvaginal suburethral slings. Porcine dermis interposition graft for restore of high grade anterior compartment defects with or without concomitant pelvic organ prolapse procedures. Use of cadaveric solventdehydrated fascia lata for cystocele repair-preliminary outcomes. Anterior restore with or without collagen matrix reinforcement: a randomized managed trial. Banked human fascia lata for the suburethral sling process: a preliminary report. Intact genetic materials is present in commercially processed cadaver allografts used for pubovaginal slings. Porcine skin collagen implants for anterior vaginal wall prolapse: a randomised prospective controlled examine. Calcification and identification of metalloproteinases in bovine pericardium after subcutaneous implantation in rats. The efficacy of Marlex mesh within the restore of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Vaginal erosion of cadaveric fascia lata following stomach sacrocolpopexy and suburethral sling urethropexy. Functional evaluation and tissue response of short- and long-term absorbable surgical meshes. Vaginal degeneration following implantation of artificial mesh with elevated stiffness. Burch colposuspension and tension-free vaginal tape within the management of stress urinary incontinence in ladies. Dynamic mechanical traits of intact and structurally modified bovine pericardial tissues. Comparison of longterm outcomes of autologous fascia lata slings with suspend tutoplast fascia lata allograft slings for stress incontinence. An examination of the biologic response to injectable glutaraldehyde cross-linked collagen implants. Colporrhaphy compared with mesh or graft-reinforced vaginal paravaginal repair for anterior vaginal wall prolapse: a randomized managed trial. Levatorplasty launch and reconstruction of rectovaginal septum utilizing allogenic dermal graft. Repair of a vaginal evisceration following colpocleisis using an allogenic dermal graft.
Discount colchisol 0.5 mg amexUrinary deposits and blood clots could obstruct the smaller-caliber catheters virus vodka generic colchisol 0.5 mg online, necessitating frequent irrigation vantin antibiotic for sinus infection buy colchisol 0.5 mg with visa. The invasive nature of insertion can lead to antibiotics in livestock buy cheap colchisol 0.5mg uncommon problems similar to hematuria antibiotic resistance can boost bacterial fitness buy 0.5mg colchisol with visa, cellulitis, bowel damage, urine extravasation, and catheter fracture. However, suprapubic catheters can be helpful in patients who bear gynecologic procedures that require long-term bladder drainage. In a recent case collection, suprapubic catheters were positioned in patients who underwent surgery for stress incontinence using mid-urethral slings. These sufferers have been in a place to measure their voiding perform and conduct voiding trials at house, which was convenient and time saving for the patients. Contraindications to suprapubic insertion, particularly closed insertion, include in depth abdominal adhesions from earlier surgeries, ventral hernia, in depth intraoperative bladder reconstruction, carcinoma of the bladder, and postoperative anticoagulation therapy. Despite these potential issues, suprapubic catheters are preferred to transurethral catheters when extended drainage is anticipated or when significant dissection across the urethra has been carried out. It is preferred when distension of the bladder is troublesome, when gross hematuria is current, when there has been a recent cystotomy, or in the presence of gynecologic malignancy. A stab incision is made through the skin above or beneath the surgical incision (the suprapubic catheter incision must be separate from the surgical incision) with a scalpel. The bladder is then punctured via the dome, taking care to avoid massive vessels. The catheter is superior via the sheath or over the needle guide, which is concurrently withdrawn. This positioning helps make certain that no bowel lies between the bladder and the anterior stomach wall. Decreased blood flow, ensuing from overdistension, is cited as one of the most common causes. The benefits of eliminating overdistension outweigh the disadvantages of intermittent insertion of a nonsterile catheter. Each catheterization event carries a 3% to 4% infection rate, and bacteriuria occurs in most sufferers inside 2 to 3 weeks. Spread the labia with the fourth and index fingers of 1 hand and use the center finger to find the urethra. Ninety percent of those kids had been freed from major kidney infection after 10 years, regardless of a 56% price of intermittent bacteriuria. The frequency of catheterization is an important issue as far as prevention of infection. Complications apart from infection are uncommon; they include retention of the catheter and perforation of the urethra to create a false passage. The patient ought to be provided with a device to measure urine and with brief plastic or rubber catheters. There are newer hydrophilic low-friction catheters that might be more comfy than the usual plastic catheters. Patients should be instructed to carry catheters at all times, with separate containers for clear and used catheters. Home sterilization with a microwave oven has been described, but whether or not this technique is of any clinical significance in preventing bacteriuria and an infection remains to be proven. Catheterization could be carried out anywhere, and the significance of emptying the bladder typically sufficient to hold the urine volumes obtained lower than four hundred to 500 mL must be careworn to the affected person. The must catheterize ought to take priority over the supply of soap and water. Voiding must be tried before each catheterization, and the residual urine quantity measured and recorded, if potential. Voiding Trials after Surgery It is widespread to have postoperative voiding dysfunction after prolapse or incontinence surgery. It is estimated that 3% to 40% of sufferers who undergo urogynecologic procedures will have postoperative voiding dysfunction. There are many components contributing to voiding dysfunction postoperatively, together with kind of anesthesia used through the surgical procedure, type of surgical procedure, analgesia used, and fluid standing of the patient. There have been a number of retrospective research which have analyzed preoperative threat elements. The voided quantity is measured and if the patient can void more than 50% of the fluid placed in the bladder, he or she can remain catheter-free. An alternate course of is to remove the catheter, permit the affected person to naturally fill his or her bladder, and then have the affected person spontaneously void. Once the patient has urinated, the residual urine within the bladder could be measured through straight catheterization or bladder scanner. A urinalysis may be accomplished and, if optimistic, cultures sent or empiric short-course antibiotics given. A research in hospitalized sufferers who underwent short-term urinary catheterization suggested that they might profit from antimicrobial prophylaxis when the catheter is eliminated, as the patients given antimicrobial prophylaxis skilled fewer subsequent urinary tract infections (Marschall et al. General Catheter Care A Foley catheter inserted transurethrally after uncomplicated surgical procedures may be removed on the first postoperative day. If the affected person has difficulty voiding, the Foley could also be changed or intermittent catheterization can be utilized till normal voiding is established. The catheter is left to straight drainage until the patient is ready to stand up and begin voiding trials. The catheter is clamped and the affected person allowed to void with the catheter clamped no less than once each 2 to 4 h. If the affected person seems to be voiding well, a postvoid residual volume may be obtained by unclamping the tube for 15 min after a voiding episode and measuring the quantity of urine obtained. When the residual volume is less than 20% to 50% of the total voided volume, the catheter can be removed. If voiding trials are unsuccessful, the patient ought to be discharged with the catheter and given written instructions and diary forms to continue the voiding trials at home. The patient ought to observe up within the office a couple of days to 1 week later, or when the postvoid residual is less than one hundred mL. These choices vary from shields resembling odd sanitary pads to disposable briefs to washable clothes designed to hold pads, in addition to menstrual sanitary pads. Absorbent products which might be disposable are probably the most commonly used devices for incontinence. Absorbent products are manufactured from many various designs; nonetheless, they are often categorized into two common groups: merchandise used for "mild" bladder management and merchandise used for "average" or "heavy" incontinence. The evaluation additionally discovered that women choose "pull-up" type protective clothes; however, these are costlier than inserts. Women with overactive bladder spend more cash on pads than girls with stress urinary incontinence. These are shaped like sanitary pads but include a powder (such as sodium polyacrylate) and a fluffed cellulose wooden pulp that absorbs liquid to type a gel, thus preventing clothes wetness. They are available in several absorbencies and are best for sufferers who expertise small quantities of urine loss.
Colchisol: 0.5 mg
References - Levey S, Jennings ER: The use of control charts in the clinical laboratory, Am J Clin Pathol 20:1059, 1950.
- Timmons JW Jr, Malek RS, Hattery RR, et al: Caliceal diverticulum, J Urol 114:6n9, 1975.
- Walczak EM, Hammer GD: Regulation of the adrenocortical stem cell niche: implications for disease, Nat Rev Endocrinol 11(1):14n28, 2014.
- Sitki-Green DL, Edwards RH, Covington MM, et al. Biology of Epstein-Barr virus during infectious mononucleosis. J Infect Dis. 2004;189:483-492.
|