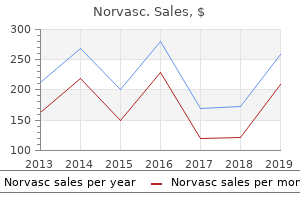
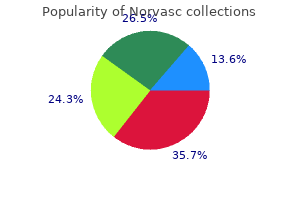
Norvasc
Jennifer M. Kalish, M.D., Ph.D. - The Children’s Hospital of Philadelphia
- Philadelphia, Pennsylvania
Discount 2.5 mg norvasc visaPrimary heart attack labs order 2.5 mg norvasc visa, secondary arrhythmia that makes you cough buy norvasc 2.5 mg online, or early latent syphilis can be handled with benzathine penicillin G hypertension gout purchase 2.5mg norvasc with mastercard, 2 heart attack water buy cheap norvasc 2.5 mg online. For late latent or latent of unknown duration syphilis, treatment consists of penicillin G 2. However, knowledge to help use of alternative regimens continues to be limited and shut comply with up is important. If compliance is of concern in penicillin-allergic individuals, then desensitization and remedy with penicillin are beneficial. Penicillin stays the one really helpful therapy in pregnancy, with enough evidence demonstrating efficacy for stopping maternal syphilis transmission to the fetus and for treating fetal an infection. Some authorities additional suggest following the beneficial or various neurosyphilis remedy with benzathine penicillin 2. Patients with a penicillin allergy in whom compliance points are of concern will due to this fact require desensitization. Titers should lower fourfold by 6 months and turn out to be nonreactive by 12 to 24 months after completion of remedy. The Jarisch-Herxheimer response is an acute febrile response incessantly accompanied by fever, chills, headache, myalgia, malaise, pharyngitis, rash, and other symptoms that often occur inside the first 24 hours (generally throughout the first eight hours) after any therapy for syphilis. This reaction was initially recognized within the remedy of neurosyphilis, however could be seen with any syphilitic therapy, most commonly with early syphilis (up to 90% of patients with secondary syphilis). The Jarisch-Herxheimer response would possibly induce preterm contractions or trigger fetal distress in pregnant girls, however this should not stop or delay therapy. Primary infections normally begin with flulike signs together with malaise, myalgias, nausea, diarrhea, and fever. Vulvar burning and pruritus precede the multiple vesicles that appear next and normally remain intact for 24 to 36 hours earlier than evolving into painful genital ulcers. After this preliminary herpes outbreak, recurrent episodes can occur as regularly as one to six times per year. It is essential to observe that subclinical or asymptomatic shedding can occur and is extra frequent in the course of the first 6 months after acquisition and immediately before or after recurrent outbreaks. Because of the potential for frequent recurrence and the devastating consequences of neonatal herpes, pregnant ladies ought to have vaginal examinations across the time of supply. Diagnosis Clinical diagnosis is often made with an examination of the vesicles and ulcers at the facet of a sexual historical past. Viral cultures are used as the gold normal for diagnosis; nonetheless, sensitivity of tradition is low, particularly in recurrent or therapeutic lesions. A Tzanck smear prepared of the lesions and examined for multinucleated big cells with a attribute appearance may reveal typical cytologic modifications, however this study can additionally be neither sensitive nor particular. Although solely about 5% of ladies report a historical past of genital herpes infection, as many as 25% to 30% have antibodies on serologic testing. Although some girls have the basic extreme presentation of genital herpes with painful genital ulcers, many ladies have a gentle preliminary presentation or are completely asymptomatic. For a main an infection, acyclovir 200 mg 5 instances per day, acyclovir four hundred mg 3 times per day, famciclovir 250 mg three times per day, or valacyclovir 1 g twice per day orally for 7 to 10 days are really helpful therapies in therapy of first medical outbreak reducing the size of an infection and the length of time a patient has viral shedding. Oral acyclovir four hundred mg three times every day or 800 mg twice day by day for five days could additionally be used for remedy of recurrent lesions. For people with frequent recurrences, prophylactic or suppression therapy of four hundred mg orally twice every day is beneficial and may cut back recurrences by 80%. Alternatively, extra pricey antiviral medicines may be used, corresponding to valacyclovir, particularly for simpler dosing regimens. The main stage of this sickness is usually a local lesion which may be both a papule or a shallow ulcer, and is often painless, transient, and can go unnoticed. The secondary stage (inguinal syndrome) happens 2 to 6 weeks after the primary lesion and is characterised by painful irritation and enlargement of the inguinal nodes (typically unilateral). Rectal exposure can result in the tertiary stage (anogenital syndrome), which is characterised by proctocolitis, rectal stricture, rectovaginal fistula, and elephantiasis (lymphatic filariasis). Initially, an anal pruritus will develop with a concomitant mucous rectal discharge. Although diagnosis is generally made per scientific suspicion, genital and lymph node specimens may be tested for C. If the exterior genitalia and rectum are disfigured and scarred, surgical measures may be required. Chancroid seems as a painful, demarcated, nonindurated ulcer positioned anywhere within the anogenital region. Usually, just a single ulcer is present, however a number of ulcers and infrequently extragenital infections have been known to occur. Other nonulcerative lesions include molluscum contagiosum, brought on by a pox virus, and lesions caused by Phthirus pubis, the crab louse, and Sarcoptes scabiei, the itch mite. Finally, when considering nonulcerative lesions, folliculitis ought to always be included within the differential analysis as a outcome of Diagnosis Diagnosis is a challenge as a outcome of H. Often, transporting the culture swab in Amies or Stuart transport media or chocolate agar can aid within the tradition. These fleshy, exophytic growths are covered with small, papillary surface projections. In rare cases, folliculitis can lead to bigger lesions such as boils, carbuncles, and abscesses. The usual supply of these infections is skin flora, primarily Staphylococcus aureus. Factors contributing to these lesions within the anogenital area embody tight undergarments, sanitary pads, poor hygiene, diabetes, and immunosuppression. An estimated 90% of genital warts are brought on by serotypes 6 and eleven, whereas cervical most cancers is more typically associated with serotypes 16, 18, and 31. Diagnosis Genital warts are usually asymptomatic but may be painful or pruritic. Initially, the lesions are small, 1 to 5 mm diameter lesions, however these can evolve into larger pedunculated lesions and ultimately into cauliflower-like growths, significantly in immunocompromised sufferers. In addition to the vulva, perineal physique, and anogenital region, these lesions can also come up in the anal canal, on the walls of the vagina, and on the cervix. When unsure of analysis or for lesions which are unresponsive to remedy, a biopsy of the lesion can be made for definitive diagnosis. Also generally identified as water warts, these lesions comprise a waxy materials that reveals intracytoplasmic molluscum bodies underneath microscopic examination when stained with Wright stain or Giemsa stain. Molluscum lesions can happen anyplace on the skin besides on the palms of the arms and soles of the ft. Diagnosis is mostly made clinically; however, diagnosis could also be confirmed with lesion biopsy for histologic or electron microscopic examination. These could be removed by way of local excision and/or therapy of the nodule base with trichloroacetic acid or cryotherapy. Treatment Treatment of the lesions contains local excision, cryotherapy, topical trichloroacetic acid, topical 25% podophyllin, and 5-fluorouracil cream (Efudex 5%).
Generic 10 mg norvasc amexContraindications to arthroscopic treatment embrace altered neurovascular anatomy blood pressure chart age group cheap 10mg norvasc overnight delivery, limited surgical expertise prehypertension co to znaczy cheap 5 mg norvasc, and superior involvement of the ulnohumeral joint hypertension pulmonary buy cheap norvasc 5mg. Open D�bridement Open d�bridement can be performed for all sufferers with primary degenerative arthritis of the elbow arteria facial buy discount norvasc 2.5mg online. Open joint d�bridement should be thought-about in patients with superior disease or when the treating surgeon has limited expertise with arthroscopic techniques. Options for open d�bridement of the elbow include: Outerbridge-Kashiwagi arthroplasty (see Chap. Several surgical options exist for the management of primary degenerative arthritis of the elbow. Surgery is directed toward addressing the pathology contributing to the predominant complaints of the affected person. These patients should have attempted and failed all different applicable remedy choices. Implant Choices Unlinked (resurfacing) and linked (semiconstrained) designs could additionally be applicable in sufferers with main degenerative arthritis of the elbow. The present literature supports the use of linked implant designs for primary degenerative arthritis. However, osteoarthritis may be the most effective indication for the use of an unlinked implant. Muscle activation about the elbow protects against extreme loading, thereby lowering aseptic loosening. Advantages of arthroscopy embrace the flexibility to visualize the entire joint and limited morbidity from surgical procedure. Savoie et al reported good results with extensive arthroscopic d�bridement involving capsular release, fenestration of the distal part of the humerus, and removal of osteophytes. Linkable implants can be utilized unlinked (B), or the ulnohumeral articulation can be captured, changing the unlinked implant to a linked implant (C). This has the theoretical, however unproven, advantage of offloading stresses on the implant. Some authors consider that this potential advantage could permit this implant kind to be used in a higher-demand patient inhabitants. Therefore, the indications for total elbow alternative are nonetheless limited on this patient population to patients keen to undertake low bodily calls for. If an unlinked implant is considered in this affected person population, the flexibility to convert to a linked replacement (linkable) has obvious advantages. Patient Positioning the patient is positioned supine on the working room table with a bump beneath the ipsilateral scapula. The use of a sterile tourniquet will increase the "zone of sterility" and permits elimination for more proximal exposure if wanted. Approach the surgical approach for linked arthroplasty is discussed in different chapters. Please check with these chapters for the particular technical particulars of implantation of a linked, semiconstrained implant. This chapter will focus on an unlinked total elbow system, which can be converted to a linked implant if required for stability. The extent of flap elevation is based on how the triceps is to be managed surgically. The ulnar nerve is recognized, protected with help of a Penrose drain, and transposed anteriorly. The common strategies of triceps administration are triceps-sparing, triceps-reflecting, and triceps-splitting approaches. Triceps-sparing approaches go away the triceps hooked up to the tip of the olecranon. The benefit of this type of strategy is that it prevents triceps weak spot postoperatively, but it sacrifices surgical publicity. Triceps-reflecting approaches subperiosteally elevate the triceps from its attachment on the ulna; it have to be rigorously reattached and guarded postoperatively. Triceps-splitting approaches violate the attachment of the triceps to the ulna yet provide the advantages of improved visualization of the joint. The medial triceps is elevated in continuity with the flexor carpi ulnaris whereas the lateral triceps is elevated in continuity with the anconeus. The medial triceps attachment to the triceps is tenuous in comparability to the lateral triceps flap, which is far more robust. Triceps-splitting strategy carried from the subcutaneous border of the ulna proximally into the triceps tendon. The medial and lateral collateral ligaments are launched from their humeral attachment and tagged for later repair. The elbow is dislocated with flexion of the joint, allowing the ulna to separate from the humerus. The medial and lateral points of the axis of rotation by way of the distal humerus are determined and an axis pin is placed via these two factors, thereby replicating the axis. The central portion of the distal humerus articulation is removed, the intramedullary canal is opened, and a rod is positioned within the intramedullary canal. The humeral canal is sequentially broached to the dimensions chosen for the articular spool. If the radial head is going to get replaced, a sagittal noticed is used to resect the radial head by way of the slicing information. The ulnar canal is opened and sequentially broached to the identical size as the selected humeral part. Component Placement Ulnar Preparation Preparation of the ulna is predicated on the flexion�extension axis of the proximal radius and ulna. Care should be taken to preserve the relationship of the trochlea and capitellar portions of the spool with the native larger sigmoid notch and radial head. If a standard ulnar element goes to be used, flexible reamers may be required to put together the ulna. Trial reduction is carried out to assess the alignment, stability, and tracking of the parts. If the components are going to be inserted unlinked, the collateral ligaments are reattached to the anatomic origin by way of the humeral implant. An accessory box stitch might be positioned through the ulna and humeral element to help the collateral ligament repair. Methylene blue is added to the cement to facilitate cement elimination if required sooner or later. Next, the offset of the distal humeral articulation with respect to the intramedullary canal is determined. The relationship between the axis of flexion�extension and the intramedullary canal is decided. Measurement guides are used to determine whether or not the offset is anterior, posterior, or impartial. Once all the holes are drilled, the cutting block is eliminated and the holes are linked with an oscillating saw.
Generic norvasc 5mg free shippingGentle vary of motion of unaffected digits is began 2 weeks after flap inset blood pressure chart video cheap norvasc 10mg online, with care taken to avoid pressure on the flap blood pressure what is normal generic 10 mg norvasc. Neurovascular island flap: the splint is changed 10 days after surgery blood pressure chart diastolic generic norvasc 2.5 mg without a prescription, when sutures could be eliminated; light lively vary of motion is started arrhythmia magnesium discount norvasc 2.5mg without a prescription, with full range of movement delayed till three weeks after surgical procedure. Long-term outcome of neurovascular palmar advancement flaps for distal thumb accidents. The restoration of sensation and function after cross-finger flaps for fingertip harm. Certain wound circumstances must be adhered to , and the ideas of grafting remain constant, regardless of the location of a wound. Isograft refers to skin harvested from an identical twin of the recipient particular person. Allograft refers to pores and skin harvested from a person of the same species as the recipient individual. Xenograft refers to the use of skin grafts from a species totally different from the recipient particular person. Due to histocompatibility mismatch, these eventually separate from the wound, except in the immunosuppressed affected person, and so present solely short-term protection. Split-thickness skin grafts contain dermis, together with a various thickness of dermis that represents less than the complete thickness of the dermis. Full-thickness skin grafts incorporate the total thickness of dermis and dermis. Donor site refers to an space from which either a split- or full-thickness pores and skin graft is harvested. Depending on the thickness of the graft, donor site remedy varies, from topical dressings, which generally are used for split-thickness pores and skin graft donor sites, to direct closure, which is the similar old methodology for addressing full-thickness skin donor defects. Skin substitutes are semisynthetic or purely artificial constructs designed to act as replacements for lost skin buildings. Their list of qualities thought of to be perfect for skin substitutes still holds true more than 20 years later: Little or no antigenicity Tissue compatibility Lack of toxicity Permeability to water vapor, as could be seen in normal skin Impenetrability to microorganisms Rapid and long-term adherence to the wound bed Capacity for ingrowth of fibrovascular tissue from the wound bed Malleability, which might permit the construct to conform to the wound mattress Inherent elasticity that might not impede movement Structural stability towards linear and shear forces Smooth floor to hinder bacterial proliferation Good to tensile energy that may enable it resist fragmentation Biodegradability Low value Ease of storage An indefinite shelf life Wound Bed Before making a choice about utilizing pores and skin grafts or a substitute, it is important to be acquainted with the characteristics of a wound bed that make it suitable for grafting. A further requirement, as quickly as d�bridement is complete, is the discount of micro organism in the wound, which often is effected via the use of a pulse lavage system. This system supplies microd�bridement of the wound mattress and may help to promote the development of wholesome granulation tissue, an ideal substrate for the support of skin graft adherence. Moreover, the vacuum-assisted closure gadget can be utilized excessive of a pores and skin graft applied to a wound and, by way of its unfavorable strain effect, restrict fluid collection beneath the graft, also serving to to guarantee contact between graft and mattress via a good distribution of stress across the interface. The lack of secondary contraction seen in full-thickness pores and skin grafts supports their use on surfaces that overlie or are juxtaposed to joints. This lack of secondary contraction helps reduce the risk of unwanted joint contracture as the grafts mature. Over broad flat surfaces, such because the dorsal or volar side of the forearm, split-thickness skin grafts perform well. Wounds that contain the glabrous surface of the hand ideally are replaced with skin that possesses the same characteristics because the adjoining pores and skin. Harvest of glabrous skin from the only of the foot or from the contralateral unhurt hand should be considered for such use. When that is the case, the arch inside the sole of the foot might yield a full-thickness glabrous pores and skin graft enough to cowl the area of the unique wound; nonetheless, the donor website then might require a pores and skin graft itself. The donor site from the arch of the foot may be grafted with nonglabrous, meshed split-thickness graft with minimal morbidity because of its minimal weight-bearing requirement. Split-thickness skin graft Traditionally preferred websites have included the anterior thighs due to the benefit of harvest and postoperative care of those areas. Another site that has favorable traits when it comes to quality of graft donor, as properly as healing of donor web site, contains the scalp. The very rich vascular provide to the scalp makes splitthickness pores and skin grafts from this web site fairly robust. If the harvest is saved inside the hair-bearing portions of the scalp, little to no donor defect could be detected as quickly as hair has grown again. Moreover, due to the excessive density of epidermal appendages in the scalp, re-epithelialization of this space is more fast than at different sites on the body. This speedy re-epithelialization helps to decrease the potential for donor deformity (ie, scarring and dyspigmentation). Harvest Skin harvest is tremendously facilitated by proper preparation of the chosen website. First, a template of the mattress to be grafted ought to be transferred to the donor web site to ensure an adequate harvest. Limiting blood loss from the harvest web site is fascinating and is definitely achieved by pre-injecting the hypodermis of the planned harvest space with an epinephrine-containing local anesthetic. If a long-acting local anesthetic corresponding to Marcaine with epinephrine is used, the affected person could have the extra advantage of extended donor site anesthesia postoperatively. As split-thickness donor websites are usually fairly painful, this could be a actual benefit and is appreciated by the patient. When a large area is deliberate for harvest, consideration must be paid to the appropriate most dosage for the local anesthetic chosen. Dilute options in these instances can present the advantages sought for these larger floor areas while nonetheless respecting the utmost allowed dosages. Microanatomy As advised earlier, the surgeon should be concerned with the microanatomic circumstances of the wound mattress. Healthy fats, muscle, paratenon, or periosteum have to be present within the base of the wound to guarantee success. Additional concerns embrace proper d�bridement of nonviable tissues from the wound mattress as well as the minimization of bacterial contamination. Donor Sites Glabrous pores and skin the only of foot within the arch, starting on the junction of glabrous and nonglabrous skin alongside the medial facet of the arch the ulnar facet of the hand, beginning on the junction of the glabrous and the nonglabrous skin alongside the ulnar aspect of the palm Full-thickness skin Redundant areas of full-thickness skin out there for harvest that keep ease of main closure of the donor defect embrace the lower abdomen, working from the anterior superior iliac spine in a delicate arc across the decrease portion of the stomach to the contralateral anterior superior iliac backbone. Depending on requirements of the recipient site, selection of full-thickness pores and skin graft can vary from the relatively hairless parts found laterally to the hirsute areas discovered centrally. Smaller areas of satisfactory full-thickness skin may be harvested from the upper internal arm. This skin, positioned on the junction of the medial biceps and triceps muscle groups, is skinny and often hairless. Among the most common are traumatic injuries, which generally result in avulsive lack of skin. Other causes embrace burn injury to the upper extremity, in addition to defects created by tumor removal. Any one of these mechanisms might result in a variety of accidents, from easy pores and skin loss to accidents of deeper constructions, together with loss of paratenon or periosteum. Skin in younger adults is thick and healthy; however, in about the fourth decade the skin begins to skinny. Despite variations in pores and skin thickness at differing anatomic locations, the general dermal-to-epidermal ratio remains comparatively fixed: about 95% dermis to 5% dermis.
Safe 2.5mg norvascThe true incidence of median nerve compression in the proximal forearm is difficult to verify hypertension and pregnancy buy norvasc 2.5 mg low cost, as is the relative contribution of the assorted potential impinging buildings blood pressure medication polygraph order norvasc 2.5mg mastercard. In cases of space-occupying lesions or scarring from trauma compressing the nerve heart attack piano generic norvasc 10mg with amex, one would expect to see sensory symptoms in addition to motor abnormalities blood pressure medication and breastfeeding buy 2.5mg norvasc mastercard. Patients affected by Parsonage-Turner syndrome often will experience a prodromal viral-type illness together with important ache for several days or even weeks before the onset of weak spot. Paresthesia in the median nerve distribution within 30 seconds is taken into account a positive check. Paresthesia in the median nerve distribution and ache in the forearm are considered a positive check. The check is believed to be in preserving with compression of the median nerve at the fibrous arcade of the flexor digitorum superficialis. Paresthesia in the median nerve distribution and pain are thought-about a optimistic take a look at. A positive finding is consistent with compression of the median nerve by the pronator teres. A constructive take a look at is assumed to be in preserving with lacertus fibrosis compression of the median nerve. Plain radiographs of the proximal forearm and elbow may reveal a supracondylar process or anatomic variation. This incision generally is related to unsightly scarring and accidents to the cutaneous nerves. Lesser incisions have been described, due to this fact; these embrace a lazy S-shape incision within the proximal volar forearm, in addition to two longitudinal,1 oblique,four and transverse6 incisions. In anterior interosseous syndrome, electrodiagnostic research will confirm denervation of the anterior interosseous muscles. Electrodiagnostic research are most dear in the prognosis of proximal median nerve compression for ruling out carpal tunnel syndrome. It is brought across the elbow flexion crease and prolonged distally for about 10 cm. Cutaneous nerve branches, including branches of the lateral brachial and medial antebrachial cutaneous nerves, are recognized and atraumatically mobilized. The existence of a ligament of Struthers and supracondylar course of can then be ascertained. It shall be essential to ligate some vessels, but it will be attainable to retract most of them. It typically is feasible to retract the whole muscle mass and follow the median nerve into the superficialis arcade. The median nerve can either move between the superficial and deep pronator heads or, less commonly, move underneath both heads. A Median nerve Lacertus fibrosis Fascia overlying superficial pronator musculature Motor branches to flexor-pronator musculature Superficial pronator teres Median nerve Flexor digitorum superficialis arch C Ligament of Struthers B (not pictured) Brachial artery Brachial vein Motor branches to flexor-pronator musculature Superficial pronator teres retracted Median nerve Superficial pronator teres released Site of pronator release Median nerve Anterior interosseous nerve Radial artery D Anterior interosseous nerve E Up to 20% of the time the deep head is absent. Anterior interosseous nerve braches to the flexor pollicis longus and flexor digitorum profundus must be protected. Use of atraumatic approach with cautious hemostasis is important to prevent postoperative scarring, with resultant pain and potential weak point. If the pronator teres tendon has been released, it must be repaired in a lengthened trend. Motor branches that go from the median nerve to the muscle tissue originating from the medial epicondyle branch from the ulnar side of the nerve. The humeral or superficial head of the pronator teres is the biggest portion of the muscle. The ulnar head or deep head is way smaller, generally absent, and mostly is deep to the median nerve. Both heads, however, have tendinous insertion websites, which may be sources of impingement. In addition, fascial connections between the heads could also be present, impinging on the median nerve. Surgical method the fibrous portion of the superficialis arcade could be released with preservation of the muscle. Palpation and visualization proximally and distally may be obtained by appropriate retraction. Extensile exposures lead to easier surgical procedure but on the expense of potential unsightly scarring and dysesthesia from cutaneous nerve harm. Judicious launch of the pronator teres limits the postoperative morbidity and reduces the restoration time. Relation to carpal tunnel syndrome Patients typically could have both carpal tunnel syndrome and a extra proximal compression, ensuing within the so-called double crush phenomenon. Some authors have implied that failed carpal tunnel syndrome is due to a misdiagnosis during which the more proximal compression of the median nerve in the forearm was not recognized. If the pronator tendon has been released, lifting and forearm rotation are restricted for four weeks. Hartz et al2 showed 28 good or glorious leads to 36 operations, but a majority of patients still had symptoms. Many, if not most, sufferers continue to be a minimum of somewhat symptomatic after surgical decompression. This might replicate persistent compression as a result of inadequate release or scarring from the surgical procedure itself. It is more probably, however, that it reflects the difficulty in making the diagnosis due to the lack of goal standards. Few studies have evaluated end result following median nerve decompression within the forearm. Olehnik et al4 and Hartz et al2 each reported results for decompression of pronator syndrome. Olehnik et al4 confirmed surgical procedure to be of benefit in 30 of 37 extremities, however 9 of 39 were unchanged and 20 had only partial reduction. Partial median nerve entrapment within the distal arm because of an adjunct bicipital aponeurosis. Symptoms could also be purely motor, purely sensory, or combined, depending on the location and reason for compression. Proximal to the wrist, the nerve gives off a big dorsal sensory branch, which supplies sensation to the dorsum of the wrist and the ulnar aspect of the hand. It is four cm in length, extending from the proximal fringe of the palmar carpal ligament to the fibrous edge of the hypothenar muscular tissues. It is bordered laterally by the hook of the hamate and the transverse carpal ligament. Zone 1, about three cm in length, is the realm proximal to the bifurcation of the ulnar nerve into motor and sensory branches. Zones 2 and three are positioned next to one another, from the point the place the ulnar nerve divides into a superficial or sensory branch and a deep motor department, to the region just beyond the fibrous arch of the hypothenar muscular tissues. The deep motor department, together with the deep branch of the ulnar artery, passes between the abductor digiti quinti and the flexor digiti quinti brevis, perforating the opponens digiti quinti. The nerve supplies the three intrinsic muscles of the small finger, the third and fourth lumbricales, the volar and dorsal interossei, the adductor pollicis, and the deep head of the flexor pollicis brevis.
Purchase norvasc 10mg without a prescriptionAfter part insertion blood pressure taking generic 2.5mg norvasc with visa, the triceps mechanism is repaired by way of bone tunnels within the ulna blood pressure of normal man norvasc 2.5 mg visa. When a sliver of bone is taken with the triceps insertion arrhythmia yahoo generic 5 mg norvasc fast delivery, transverse tunnels are made pulmonary hypertension 60 mmhg generic norvasc 10 mg line. Each limb of nonabsorbable suture is tied over the top of the triceps and bone fragment. An extra cerclage suture is brought by way of one of many two transverse tunnels and is introduced across the tip of the olecranon, incorporating the triceps insertion. Regardless of the treatment undertaken, the aim of treatment is a pain-free, useful arc of motion. Goals of treatment Interposition arthroplasty Predictors of poor consequence: Painful, cellular elbow Preoperative instability Need to reconstruct both the medial and lateral ulnar collateral ligaments on the time of interposition Maintain the fixator for a minimal of four weeks (preferably 6 weeks). Patients are seen at 10 to 14 days postoperatively for staple elimination and wound verify and every 2 weeks thereafter until pin removing. The external fixator is left in place for about four to 6 weeks and then removed within the operating room with evaluation of elbow stability and movement under anesthesia. I prefer to wait 6 weeks to permit collateral ligament therapeutic since instability is the commonest complication after fixator removal. Restrictions: Lifetime limitations of the operated extremity embody 2- to 5-pound repetitive lifting and 10-lb single-event restriction. Cheng and Morrey2 found that 67% of sufferers handled for rheumatoid arthritis had satisfactory relief of ache, and 75% of patients treated for osteoarthritis had been happy at 5-year follow-up. Total Elbow Replacement the elbow is immobilized in full extension in a well-padded anterior splint. Mechanical issues such as component fracture and increased polyethylene bushing wear are more common. Treatment of the cell, painful arthritic elbow by distraction interposition arthroplasty. Salvage of non-union of supracondylar fracture of the humerus by whole elbow arthroplasty. Results of total elbow arthroplasty as a salvage process for failed elbow reconstructive operations. Intrinsic constraint of unlinked whole elbow replacements: the ulnotrochlear joint. Interposition arthroplasty with an Achilles tendon allograft as a salvage process for the elbow. Total elbow arthroplasty in the treatment of posttraumatic situations of the elbow. Interposition arthroplasty of the elbow with hinged external fixation for post-traumatic arthritis. Semiconstrained total elbow alternative for the remedy of post-traumatic osteoarthrosis. Higher infection rates are famous with posttraumatic arthritis and a history of prior surgery. Loosening Triceps insufficiency (an underrecognized problem) Neurologic damage (incidence of transient ulnar neuropathy as high as 26% and permanent nerve injury as a lot as 10%) Wound complications Associated with prior surgery Manage wound by immobilizing in extension postoperatively; use a subcutaneous drain to keep away from hematoma formation. Periprosthetic fracture (can happen intraoperatively or postoperatively; incidence ranges from 1% to 23%) Chapter 49 Elbow Arthrodesis Mark A. Arthrodesis must be thought-about a salvage process when no different satisfactory surgical option exists. The surgeon should evaluate the necessity for bone graft or soft tissue coverage earlier than arthrodesis. If soft tissue protection is necessary, a plastic surgery session is beneficial. Preoperative Planning the most effective elbow position is controversial, although the literature suggests between forty five and a hundred and ten levels. Factors for choosing the most effective place embrace: Gender Occupation Hand dominance Functional requirements Associated joint involvement Unilateral versus bilateral arthrodesis Patient preference One to 3 weeks earlier than surgery, the elbow to be fused is braced or casted in various angles. Generally acceptable angles embody: Male: dominant arm at ninety degrees Females seem to prefer lower angles of forty to 70 degrees. Bilateral elbow arthrodesis: dominant arm at a hundred and ten degrees, nondominant arm at sixty five degrees Soft tissue protection is evaluated. If gentle tissue coverage is required, the joint is stabilized with an external fixator. The surgeon ought to contemplate bulk graft with demineralized bone matrix and cancellous allograft or autograft. If an infection is suspected: Blood work is obtained for full blood count, sedimentation fee, and C-reactive protein. High-speed burr Power drill Osteotomes Oscillating saw Kirschner wire set Special Instruments Patient Positioning A tourniquet is positioned as high on the arm as possible. The affected person is placed within the lateral decubitus place with the operative arm resting on a padded arm rest. Identify neurovascular buildings in identified areas earlier than following constructions by way of areas of heavy scar tissue. Contour the bone in order that it can be decreased at the appropriate angle chosen for arthrodesis. It is usually essential to excise the radial head to permit for enough reduction of the humerus and ulna. The plate is pulled right down to the bone and secured with cortical screws before adding locked screws. Check the position and fixation of the assemble intraoperatively with fluoroscopy. This is a multiplanar cut and may accommodate for the elbow place in both the coronal and sagittal planes. Intraoperative use of a goniometer to verify the fusion angle before definitive fixation. Provisional fixation is obtained with Kirschner wires and the fusion place is measured with a goniometer. Keep sufferers in a cast for at least four months, till fusion happens, relying on radiographs. Intravenous antibiotics are continued for forty eight hours or longer, depending on intraoperative cultures. The effect of simulated elbow arthrodesis on the flexibility to perform actions of every day dwelling. Lateral plantar nerve Plantar Fascia Release in Combination With Proximal and Distal Tarsal Tunnel Release 3911 Chapter 58 Endoscopic Plantar Fasciotomy 3920 Chapter 59 Transection and Burial of Neuromas of the Foot and Ankle 3925 Chapter 60 Barrier Procedures for Adhesive Neuralgia 3933 Chapter 61 Distraction Arthroplasty for Ankle Arthritis 3941 Chapter 62 Supramalleolar Osteotomy With Internal Fixation: Perspective 1 3953 Chapter 63 Supramalleolar Osteotomy With Internal Fixation: Perspective 2 3961 Chapter 64 Supramalleolar Osteotomy With Internal Fixation: Perspective 3 3967 Chapter 65 Supramalleolar Osteotomy With External Fixation: Perspective 1 3976 Chapter sixty six k. The chevron osteotomy has turn into extensively accepted for correction of delicate and reasonable hallux valgus deformities. In the initial reports by Austin and Leventen1 and Miller and Croce,thirteen no fixation was mentioned. They instructed that the form of the osteotomy and impaction of the cancellous capital fragment upon the shaft of the primary metatarsal provided adequate stability to forego fixation. To enhance the indication for this technically easy osteotomy, inner fixation and a lateral delicate tissue release have been added.
Purchase norvasc 5mg with mastercardThe patient is placed in a supine position on the working desk with a rolled towel beneath the ipsilateral scapula heart attack facts discount norvasc 5 mg on-line. The complete operative extremity and shoulder girdle is prepared and draped; a sterile tourniquet is placed hypertension 39 weeks pregnant generic 5mg norvasc overnight delivery. Approach Although a number of approaches may be used heart attack racing order 5mg norvasc visa, the BryanMorrey method (triceps�anconeus "slide") is preferred hypertension malignant generic norvasc 2.5 mg mastercard. The ulnar nerve is carefully identified and isolated along the medial side of the triceps. The intermuscular septum is excised and a deep pocket of subcutaneous tissue over the flexor pronator group distally and anterior to the triceps proximally is created. The nerve is then anteriorly transposed into this subcutaneous tissue pocket; it should be protected throughout the operation. The tip of the olecranon is removed with a rongeur or oscillating saw, relying on the standard of the bone, and the humerus is then externally rotated and the elbow fully flexed to adequately expose the articulating surfaces of the humerus, ulna, and radial head. The ulnar nerve is recognized along the medial border of the triceps, and a vessel loop is positioned. Under rigidity, the medial and ulnar border of the triceps (C) and the anconeus (D) are incised from their insertions into the olecranon. The medial collateral ligament is released to give the elbow maximal movement and to facilitate complete publicity of the ulnohumeral joint. For patients with severe stiffness, the effect of humeral shortening should be thought-about. Hughes et al4 developed a biomechanical model that demonstrated that resecting 1 cm or much less of humeral bone has little effect on triceps energy. With the elbow in 30 degrees of flexion, resecting 1 to 2 cm lowered triceps energy by 17% to 40%, while shortening of 3 cm lowered extension energy by 63%. With the midportion of the trochlea eliminated, a thin rasp or intramedullary information is used to again determine the humeral canal. The anterior capsule is completely subperiosteally launched from the anterior facet of the humerus to accommodate the flange of the humeral element and to permit unencumbered postoperative elbow extension. The humeral slicing jig is aligned as a template for removing of the distal humeral articulation. An oscillating noticed is positioned at an oblique angle to the jig to precisely remove the articulating floor of the distal humerus while avoiding cross-hatching of the supracondylar columns. Again, a twist reamer is used to further establish the canal, and an appropriately sized ulnar rasp is then inserted. The ulnar bow must be acknowledged and palpated whereas inserting the ulnar rasps to keep away from ulnar perforation. This could also be performed by rotating the forearm and utilizing a rongeur to progressively excise the radial head from an axial orientation, whereas holding the elbow in full flexion. A small twist reamer is used to determine the ulnar canal (C), which is then rasped to the suitable size whereas sustaining correct rotation (D). Range of motion is tested and ought to be full with out limitation within the flexion�extension aircraft. If vary of movement is limited owing to inadequate delicate tissue release, this should be addressed presently. Based on the trial components used, the length of the cement applicator is measured to equal that of the humeral part. Two packs of cement with antibiotics are mixed and injected with a runny consistency. The humeral cement is placed first, adopted by the ulnar cement and then the ulnar component. The elbow is taken through several arcs of flexion�extension to "normalize" the rotational version of components to each other. The ulnar and humeral elements are linked by two interlocking cross-pins, that are placed from opposite sides. A slight bow could additionally be created in the proximal aspect of the humeral component if humeral bowing or a small canal is current. The elbow is flexed to about 60 degrees and the extensor mechanism is reduced over the tip of the olecranon; consider slightly overreducing the extensor mechanism medially to decrease the potential for postoperative lateral subluxation. These suture ends are then handed again via the forearm extensor fascia and tied collectively. Two reinforcing sutures are then handed via the transverse holes and extensor fascia earlier than being tied together. Suture is passed by way of the proximal ulna and then woven through the triceps tendon earlier than being tied together. A volar splint is positioned with the elbow in full extension, making sure to adequately pad the anterior facet of the splint both proximally and distally to stop pores and skin breakdown. This contains full releases of the lateral ulnar collateral ligament and medial collateral ligament complexes, and an entire anterior capsule launch. Consider reflection of widespread flexors or extensors if severe deformities or arthrofibrosis is current. Humeral preparation Shorten the humerus by 1 cm or much less to augment postoperative range of movement without compromising strength. Use a burr distally to open up the humeral canal if wanted, quite than forcing with rasps. Always palpate the ulna and contemplate the ulnar bow before ulnar preparation to avoid perforation. The drain is removed on postoperative day 1 or when output is less than 30 mL in an 8-hour period. The patient is restricted to no pushing and no overhead actions for three months to protect the triceps. In addition, no repetitive lifting of objects heavier than 5 kilos and no lifting greater than 10 pounds in a single occasion is allowed for life. The mean flexion�extension arc of movement improved by only 27 degrees (from 67 to ninety degrees) in this research, but these outcomes had been reported before shortening of the humerus for severely contracted elbows was routinely carried out. The Mayo Elbow Performance Score assigns numeric values to every of those categories to produce scores for each of these standards in addition to an general score. Reduction of triceps muscle force after shortening of the distal humerus: a computational mannequin. The key level in determining how to deal with acute elbow fractures is to assume that every one fractures will be anatomically decreased and glued. An acute elbow replacement ought to be thought of solely whether it is felt that open reduction and inner fixation is unlikely to obtain a predictably good practical consequence. In the vast majority of instances, elbow replacements for the therapy of acute fractures should be limited to the physiologically aged affected person with low demands and osteoporotic bone stock. A full examination of the elbow must also embrace analysis of associated injuries.
Diseases - Strumpell Lorrain disease
- Cerebellar agenesis
- Antiphospholipid syndrome
- Enchondromatosis dwarfism deafness
- Posterior valve urethra
- Ohdo Madokoro Sonoda syndrome
- Eosinophilic fasciitis
Norvasc: 10 mg, 5 mg, 2.5 mg
Discount norvasc 2.5 mg with mastercardThe forearm is rotated to acquire a circumferential view of the fracture and appreciate the secure zone for hardware placement arteriogram complications norvasc 10mg generic. If comminution (more than three pieces) is clear at this step normal blood pressure chart uk buy discount norvasc 10mg online, we elect to exchange the radial head blood pressure good average purchase norvasc 10mg online. The fragments are reduced provisionally with a tenaculum and held with small Kirschner wires placed out of the zone the place definitive fixation is planned blood pressure danger zone chart cheap 10mg norvasc with mastercard. Drill holes with transosseous sutures are a confirmed technique, however most authors now use suture anchors with reproducible outcomes. We have a low threshold for excision or arthroplasty in the setting of comminution. A fluoroscopy unit ought to be obtainable for examination beneath anesthesia earlier than sterile preparation. Prosthetic radial head substitute ought to be mentioned with the affected person as an option and ought to be available within the room ought to the fracture show to be comminuted. Examination A thorough fluoroscopic examination is an important factor in deciding what therapy is appropriate. To get hold of a true lateral we recommend abducting the arm and externally rotating the shoulder while inserting the elbow on the image intensifier. Light activities of day by day dwelling are allowed at 2 weeks, with increased weight bearing at 6 weeks. Complications and resultant secondary procedures shall be more likely in circumstances with undiagnosed instability and associated damage. Although these lowprofile implants had been apparently properly placed, this patient went on to develop avascular necrosis with fragmentation of the radial head. Infection Early and late instability from missed or failed remedy of associated injuries the rate of avascular necrosis is about 10%, significantly greater in displaced fractures. This is expected provided that the radial recurrent artery inserts in the protected zone where hardware is placed. Primary nonoperative remedy of moderately displaced two-part fractures of the radial head. Surgical publicity of the ulna and proximal third of the radius via one incision. The nonarticulating portion of the radial head: Anatomic and scientific correlations for inside fixation. Comminuted fractures of the radial head: comparison of resection and internal fixation. Reliability analysis of classifying radial head fractures by the system of Mason. Radial head arthroplasty is indicated for unreconstructable displaced radial head fractures with an associated elbow dislocation or a known or possible disruption of the medial collateral, lateral collateral, or interosseous ligaments. Biomechanical studies have proven that the kinematics and stability of the elbow are altered by radial head excision, even within the setting of intact collateral ligaments,15 and are improved with a metallic radial head arthroplasty. Injuries of the medial collateral or lateral collateral ligament or the interosseous ligament are sometimes related to comminuted displaced unreconstructable radial head fractures. Metallic radial head alternative in elbows with intact ligaments restores the kinematics and stability similar to that of a native radial head and has been proven to present good scientific and radiographic end result in most patients at medium-term follow-up; nevertheless, long-term end result studies are lacking. The articular dish has an elliptical shape that varies considerably in size and shape and is variably offset from the axis of the radial neck. There is a poor correlation between the size of the radial head and the medullary canal of the radial neck, making a modular implant desirable for an optimum match. The radial head is an important valgus stabilizer of the elbow, significantly in the setting of an incompetent medial collateral ligament, which is the primary stabilizer against valgus drive. The radial head can additionally be important as an axial stabilizer of the forearm and resists varus and posterolateral rotatory instability by tensioning the lateral collateral ligament. Axial, valgus, and posterolateral rotational patterns of loading are all thought to be doubtlessly answerable for these fractures. The lateral ulnar collateral ligament is an important stabilizer against varus and posterolateral rotational instability of the elbow and ought to be preserved or repaired after radial head arthroplasty. Careful palpation of the radial head, the medial and lateral collateral ligaments of the elbow, the interosseous ligament of the forearm, and the distal radioulnar joint should be carried out. Local tenderness over one or all of these structures implies a possible derangement of the relevant construction. Since associated injuries of the shoulder, forearm, wrist, and hand are widespread, these areas must be carefully examined. Range of motion, including forearm rotation and elbow flexion�extension, ought to be evaluated. Loss of terminal elbow flexion and extension is expected as a consequence of a hemarthrosis in acute fractures, while loss of forearm rotation typically is brought on by a mechanical impingement. A cautious neurovascular assessment of all three major nerves that cross the elbow must be performed. The examiner should evaluate lively and passive vary of motion to the uninjured aspect. Reduced range of movement may be a results of hemarthrosis or mechanical block from a damaged fragment. Intra-articular injection of a neighborhood anesthetic helps differentiate between decreased vary of motion as a end result of a mechanical block versus pain inhibition. Fragment size, number of fracture fragments, degree of displacement, and bone high quality influence choice making concerning the optimal administration. Nondisplaced fractures or small (less than 33% of radial head) minimally displaced fractures (less than 2 mm) can be treated with early movement with an excellent outcome within the majority of patients. Associated injuries and a block to motion are also essential components to consider when deciding between nonoperative and surgical management. Radial head fractures which are displaced however too comminuted to be anatomically reduced and stably fixed and that are too giant to contemplate fragment excision (involve more than 1 / 4 to a third of the radial head) must be managed by radial head excision with or without arthroplasty. The determination as to what fracture is reconstructable is dependent upon surgeon components (eg, experience), patient components (eg, osteoporosis), and fracture components (eg, fragment quantity and measurement, comminution, related gentle tissue injuries). Other indications for radial head arthroplasty include radial head nonunion or malunion, main or secondary management of forearm or elbow instability (eg, Essex-Lopresti injury), rheumatoid arthritis or osteoarthritis, and tumors. Preoperative Planning Currently obtainable gadgets embrace spacer implants, press-fit and ingrowth stems, and bipolar and ceramic articulations. Silicone radial head implants supply little in the method in which of axial or valgus stability to the elbow and have been difficult by a high incidence of implant put on, fragmentation, and silicone synovitis resulting in generalized joint damage. Most metallic radial head implants which have been developed and used to date employ a monoblock design, making dimension matching suboptimal and implant insertion usually difficult due to the necessity to subluxate the elbow to permit for insertion of these devices. Preoperative 3D reconstruction pictures demonstrating a comminuted radial head fracture with a small undisplaced coronoid fracture. Precise implant sizing and placement are important with these units to guarantee appropriate capitellar tracking and to keep away from a cam impact with forearm rotation, which may cause premature capitellar wear as a result of shearing of the cartilage and stem loosening as a outcome of elevated loading of the stem�bone interface. Positioning the affected person is positioned supine on the operating table and a sandbag is positioned beneath the ipsilateral scapula to help in positioning the arm throughout the chest.

Discount 5mg norvasc with amexA thorough neurovascular examination have to be carried out and deficits evaluated with angiography and electromyography blood pressure 210120 buy norvasc 5 mg fast delivery, as essential blood pressure chart 13 year old cheap 5 mg norvasc overnight delivery. A thorough delicate tissue examination also is warranted arteria carotis communis discount 10mg norvasc mastercard, as wounds might symbolize an open fracture and warrant exploration blood pressure chart vs age 2.5 mg norvasc free shipping. In addition, the bony relationships ought to be evaluated for evidence of any ligamentous disruption. Glenoid neck fractures with more than forty levels of angulation within the coronal or sagittal aircraft or translational displacement of 1 cm or extra require surgical administration. Anatomic neck fractures (lateral to the coracoid process) are inherently unstable and must also be considered for operative intervention. Significant displacement or fractures at the side of other bony and delicate tissue injuries to the shoulder girdle could require surgical stabilization. The shoulder girdle is prepped and draped extensively, and the whole upper extremity is prepped and draped "free. A superior approach can added for control and positioning of a difficult-to-control glenoid fragment. The lateral decubitus position is used for posterior and posterosuperior approaches to the glenoid process. An incision is made alongside the scapular backbone and acromion and down the lateral aspect of the shoulder, as wanted. Mobilization of the teres minor muscle allows entry to the lateral scapular border. The standard posterior incision extends along the inferior margin of the scapular spine and the acromion. At the lateral tip of the acromion, the incision continues within the midlateral line for two. The posterior and middle heads of the deltoid muscle have been indifferent from the scapular spine�posterior acromial process and retracted distally to expose the infraspinatus musculotendinous unit. The infraspinatus�teres minor interval has been developed, with the infraspinatus retracted superiorly and the teres minor retracted inferiorly to expose the posterior glenohumeral joint capsule (the inferior portion of the infraspinatus insertion has been released). The infraspinatus tendon and underlying posterior glenohumeral joint capsule are incised 2 cm from insertion on the larger tuberosity to permit entry to the glenohumeral joint. Care must be taken to keep away from violating the glenoid fossa with the screws within the glenoid fragment. Meticulous restore of the deltoid origin to the scapular spine�acromion ought to be performed with permanent sutures by way of drill holes. Standard anterior incision extends from the superior to inferior margin of the humeral head, centered over the glenohumeral joint. Most nonarticular injuries and all scapular body�spine fractures are treated nonoperatively. Approach Deltoid detachment and reflection supplies maximal visualization and is recommended for surgeons unfamiliar with the posterior method. During the posterior strategy, the internervous aircraft is between the infraspinatus (a bipennate muscle) superiorly and the teres minor inferiorly. Reduction Fixation K-wires may be positioned to serve as "joysticks" to help with fracture discount. However, they are often placed percutaneously and used for momentary or supplemental fixation, being removed at four to 6 weeks. Closure Meticulous restore of the deltoid to the scapular spine�acromial course of is necessary, using nonabsorbable sutures positioned through drill holes. Progressive passive and active-assisted vary of movement exercises are emphasised throughout weeks 2 via 6 postoperatively. Strengthening is begun after 6 weeks postoperatively and after range of motion is passable. While most nonarticular scapular fractures are treated nonoperatively, people who warrant surgical intervention seem to benefit from this treatment. The musculocutaneous and axillary nerves are vulnerable within the anterior method, the suprascapular nerve within the superior strategy, and the axillary and suprascapular nerves in the posterior method. Chapter 23 Open Reduction and Internal Fixation of Intra-articular Scapular Fractures Brett D. Over 90% of fractures of the glenoid cavity are insignificantly displaced and are managed nonoperatively. In addition, the bony relationships should be evaluated for evidence of ligamentous disruption(s) or instability. The glenoid course of consists of the glenoid cavity (the glenoid rim and glenoid fossa) and the glenoid neck. The glenoid cavity supplies a agency concave surface with which the convex humeral head articulates. They are true fractures, not avulsion injuries attributable to oblique forces utilized to the periarticular gentle tissues by the humeral head. Fractures of the glenoid fossa happen when the humeral head is driven into the center of the concavity. The fracture then promulgates in numerous different instructions, depending on the traits of the humeral head pressure. Significantly displaced glenoid fossa and glenoid rim fractures require operative administration. Significant displacement may find yourself in posttraumatic degenerative joint illness, glenohumeral instability, and even nonunion. The superior method is used, along side a posterior method, for fractures of the glenoid fossa with a difficultto-control superior fragment. The anterior approach is used for fractures of the anterior glenoid rim and some fractures involving the superior side of the glenoid fossa. Origins of the posterior and middle heads of the deltoid muscle are sharply indifferent from the scapular spine� acromial process, and the deltoid muscle is split in the line of its fibers for two. Subperiosteal mobilization of the teres minor muscle allows entry to the lateral scapular border. The posterior and posteromedial heads of the deltoid are indifferent from the scapular backbone and acromial process. The infraspinatus tendon and underlying posterior glenohumeral capsule are incised 2 cm from insertion on the higher tuberosity to permit entry to the glenohumeral joint. The trapezius and underlying supraspinatus muscle tissue are break up according to their fibers. The deltoid muscle is cut up within the line of its fibers over the palpable coracoid process and retracted medially and laterally. Incise the anterior glenohumeral capsule in the identical style, tag its corners, and turn it back medially to acquire entry to the glenohumeral joint. Incise the subscapularis tendon 2 cm from its insertion on the lesser tuberosity, dissect it off the glenohumeral capsule, incise the capsule equally, and turn both of them back medially to gain entry to the glenohumeral joint. All delicate tissues divided to gain access to the fracture site have to be meticulously repaired. With posterior approaches, the deltoid must be securely reattached to the acromion and scapular spine with permanent sutures via drill holes. Axillary radiograph displaying the glenoid cavity fragments secured along with cannulated screws and the glenoid unit secured to the scapular physique with a malleable reconstruction plate (the acromial fracture was decreased and stabilized with a tension band construct).
Cheap norvasc 5 mg visaA commercially obtainable pain pump could additionally be used to augment postoperative analgesia and to scale back narcotic medication use heart attack ne demek discount 5 mg norvasc with mastercard. The affected person is then positioned in a sling or shoulder immobilizer with forty five degrees of abduction for consolation blood pressure chart of human body cheap 5mg norvasc with mastercard. Check the peak of the trial stem before performing cement fixation prehypertension during third trimester discount norvasc 5 mg without a prescription, utilizing a fracture jig or sponge for provisional fixation blood pressure medication types cheap norvasc 10 mg mastercard. Avoid loss of exterior rotation or inside rotation with overreduction of the lesser and higher tuberosities, respectively. On postoperative day 1, provoke light pendulum exercises, with passive forward flexion and exterior rotation (at 0 levels of abduction). Always modify rehabilitation protocol based on intraoperative assessment of soft tissue compromise and patient neurologic standing. When tuberosity therapeutic is obvious, part 2 workouts are initiated with isometric rotator cuff workout routines and energetic assisted elevation with the pulley. At 3 months, strength coaching with graduated rubber bands (phase 3) is carried out. In patients with chronic fractures treated with hemiarthroplasty, the most common problems encountered were instability, heterotopic ossification, tuberosity malunion or nonunion, and rotator cuff tears. Operative therapy of malunion of a fracture of the proximal side of the humerus. Tuberosity malposition and migration: purpose for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. Outcome after main and secondary hemiarthroplasty in aged sufferers with fractures of the proximal humerus. Evaluation and administration of valgus impacted four-part proximal humerus fractures. Factors that portend a poor consequence after hemiarthroplasty for fractures embody tuberosity malposition, superior migration of the humeral prosthesis, stiffness, persistent pain, poor preliminary positioning of the implant (excessive retroversion, decreased height), and age over seventy five years in girls. The normal glenohumeral relationships: An anatomical examine of one hundred and forty shoulders. Orthopaedic Trauma Association Committee for Coding and Classification: Fracture and Dislocation Compendium. Retroversion of the proximal humerus in relationship to the prosthetic substitute arthroplasty. Proximal humeral alternative for complex fractures: Indications and surgical technique. These injuries are most commonly handled nonoperatively with a prefabricated fracture brace. Patients usually can tolerate as a lot as 20 degrees of anterior angulation, 30 levels of varus angulation, and 3 cm of shortening without important functional loss. There are, nonetheless, several indications for surgical remedy of humeral shaft fractures: Open fracture Bilateral humeral shaft fractures or polytrauma; floating elbow Segmental fracture Inability to maintain acceptable alignment with closed remedy (ie, angulation greater than 15 degrees)-seen extra generally with transverse fractures Humeral shaft nonunion Pathologic fractures Arterial or brachial plexus harm Open reduction with internal plate fixation requires extensive dissection and operative skill. Injuries with high levels of power typically result in a larger diploma of fracture comminution. Indirect injuries, such as those that may occur with activities corresponding to arm wrestling, usually contain a twisting mechanism and result in a spiral fracture sample. Higher-energy accidents could lead to muscle interposition between the fracture fragments, which might inhibit reduction and healing. A research of 240 humeral shaft fractures revealed radial nerve palsies in forty two sufferers, for an total rate of 18% (17% in closed injuries). Fractures within the midshaft had been extra more doubtless to have concomitant radial nerve palsy. Twenty-five of these sufferers had full restoration in a spread of 1 day to 10 months. Median and ulnar nerve palsies were seen very hardly ever in sufferers with open fractures. The most common treatment technique is preliminary splinting from shoulder to wrist, followed by software of a prefabricated fracture brace when the patient is comfortable, usually within 2 weeks of the harm. Studies by Sarmiento and coauthors10,eleven have shown the effectiveness of practical bracing in the therapy of humeral shaft fractures. Nonunion charges with this methodology of treatment are in the 4% range, lower than seen when treating with exterior fixators, plates, or intramedullary nails. Closed fractures with initial radial nerve palsy can be observed, with anticipated restoration over a period of three to 6 months. If the scenario dictates therapy, bodily remedy reliably restores joint movement in these patients. Relative contraindications to closed treatment include bilateral humeral shaft fractures or sufferers with polytrauma who require an intact brachium to ambulate. Transverse fractures and those with vital muscle imposition are also more amenable to operative fixation. The radial nerve and profunda brachial artery pass by way of the triangular interval (bordered superiorly by the teres major, medially by the medial head of the triceps, and laterally by the humeral shaft). The nerve then transverses from medial to lateral behind the humeral shaft and travels distally to a location between the brachialis and brachioradialis muscle tissue. The musculocutaneous nerve lies on the undersurface of the biceps muscle and terminates distally because the lateral antebrachial cutaneous nerve. Proximal and midshaft fractures are more amenable to plating on the anterolateral floor, whereas distal fractures usually require posterior plate fixation. The affected person often braces the affected limb to his or her side, making analysis of shoulder and elbow range of motion difficult. Bony prominences should be gently palpated to consider for other accidents, corresponding to an olecranon fracture. Evaluate the appearance and skeletal stability of the forearm to rule out the presence of a co-existing both-bone forearm fracture ("floating elbow"). This finding necessitates operative fixation of humeral, radial, and ulnar fractures. Determine the vascular standing of the higher extremity by palpating the radial and ulnar pulses at the wrist. This construction is at risk proximally as it passes posterior to the humeral shaft after emerging from the triangular interval, in addition to distally, because it lies adjoining to the supracondylar ridge (near the situation of the Holstein-Lewis distal one-third spiral humeral shaft fracture). Examine sensory operate within the first dorsal internet area, wrist extension, and thumb interphalangeal joint extension to decide the functional standing of the radial nerve. The brace usually requires frequent retightening over the first 2 weeks as swelling subsides. Anatomic alignment of the humerus rarely is achieved, with varus deformity commonest.
Generic norvasc 5mg onlineRadiographs are used to determine whether or not the fracture is a two- hypertension 1 and 2 discount 10 mg norvasc with mastercard, three- blood pressure medication drug test norvasc 5mg with mastercard, or four-part fracture and to assess the degree of displacement blood pressure medication given during pregnancy order 2.5 mg norvasc with amex. Elderly people typically sustain proximal humerus fractures as the results of low-energy injuries such as slipping and falling hypertension of the knee norvasc 5mg. These injuries often are very amenable to minimally invasive fixation techniques, as a result of the displacement is manageable and the periosteal sleeve between fracture fragments typically is undamaged. The Y lateral view often permits the examiner to detect any posterior displacement of refined greater tuberosity fractures. The bone might not hold the pins and screws nicely and could also be higher handled with a extra secure assemble. Fractures with a comminuted larger tuberosity require suture fixation through the tendon�bone junction (required open approach). Comminution of the medial calcar region results in unstable reduction of the head onto the shaft. This process ought to be performed solely in patients dedicated to consistent follow-up within the postoperative interval. Pin migration is possible and should be caught early so as to avoid potential harm to thoracic structures. The pectoralis major muscle exerts an anterior pressure on the shaft, leading to anterior displacement of the shaft relative to the humeral head. Historically, 1 cm of displacement has been used because the criterion for clinically vital tuberosity displacement. Recently, nonetheless, even 5 mm of displacement has been considered an operative indication. Patients wear a sling for 2 to 3 weeks or till the proximal humerus feels stable with gentle inner or exterior rotation of the arm. This image should be checked before prepping and draping to confirm adequate visualization. Instruments can be launched via this portal to lever fracture fragments or pull fragments into reduced place. By sweeping posterior and superior, the higher tuberosity and its extent of displacement could be palpated. In three- and four-part fractures, the fracture line of the larger tuberosity is reliably zero. Therefore, the reduction portal is situated at the stage of the surgical neck and 1 cm posterior to the biceps groove. The C-arm is brought in parallel to the affected person, leaving the lateral facet of the arm free for instrumentation. The affected person should be positioned laterally on the table such that an enough fluoroscopic view could be obtained. The C-arm fluoroscope is positioned parallel to the patient, extending over the shoulder from the cephalad path. This position leaves the lateral shoulder utterly accessible for instrumentation and pin fixation. The discount portal is positioned on the level of the surgical neck fracture approximately 0. A hemostat is applied to the skin (C) and then imaged (D) to verify that this portal shall be instantly at the level of the surgical neck fracture. A small incision is made in the pores and skin, and the deltoid is spread bluntly to avoid injury to the underlying axillary nerve. The location of the biceps tendon is estimated based on surface anatomic landmarks. Subcutaneous tissues and the deltoid muscle are unfold bluntly using a straight hemostat to avoid harm to the axillary nerve on the deep floor of the deltoid. An axillary or scapular Y radiograph is critical to evaluate the extent of this displacement. Longitudinal traction is utilized to the arm, and a posteriorly directed pressure is applied to the proximal shaft of the humerus. A blunt instrument may be inserted into the fracture on the surgical neck to lever the head again onto the shaft. This maneuver is normally a highly effective discount device, however care should be used to avoid further harm or fracture to the humeral head throughout this maneuver, particularly on osteopenic patients. The lengthy head of the biceps tendon can turn out to be interposed between the fracture fragments, precluding reduction. Pins must be easy to keep away from injury to soft tissue upon insertion, and terminally threaded to avoid backing out. The pins should enter at different instructions to improve stability of fixation construct. One pin should enter lateral to the biceps in a primarily anterior-to-posterior direction. Another pin ought to enter additional laterally in a primarily lateral-to-medial course. Stability ought to be checked underneath fluoroscopic imaging with stay, gentle inner and exterior rotation. The start line for the pins is approximately 5 to 6 cm distal to the surgical neck fracture line. Often a posterior vector should be utilized to the shaft or an instrument could be introduced through the reduction portal to lever the top again onto the shaft. Retrograde pins are launched several centimeters below the level of the surgical neck fracture into the pinnacle. The pins ought to be placed in numerous directions to present stability to the assemble. The pins must be reduce below the pores and skin after insertion to forestall pin website infection. They are simply eliminated a few weeks later with a small process in the office or operating room. Any suggestion of instability or motion on the fracture is an indication for open discount and plate fixation at that point. The rotator cuff pulls the tuberosity medially (to a sure extent) and posteriorly. Posterior displacement and rotation typically are underappreciated and must be thought-about. The guidewire is handed through the tuberosity, throughout the surgical neck fracture, and engages the medial cortex of the proximal humeral shaft. A small incision is made over the greater tuberosity, and a cannulated screw is used for fixation. The guidewire is aimed to interact the larger tuberosity fragment as well as the medial cortex to present compression. Over-tightening must be prevented to forestall fracture of the higher tuberosity fragment. If the larger tuberosity fragment is massive sufficient, a second cancellous screw is directed by way of the tuberosity fragment, participating cancellous bone of the humeral head.
References - Launer LJ, Ross GW, Petrovitch H, Masaki K, Foley D, White LR, Havlik RJ. Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol Aging 2000;21(1):49-55.
- Ho HS, Frey CF: Gastrointestinal and pancreatic complications associated with severe pancreatitis. Arch Surg 130:817, 1995.
- Jerrett M, Shankardass K, Berhane K, et al. Traffic-related air pollution and asthma onset in children: a prospective cohort study with individual exposure measurement. Environ Health Perspect 2008; 116: 1433-1438.
- Nesterova G, Gahl WA: Cystinosis: the evolution of a treatable disease, Pediatr Nephrol 28(1):51-59, 2013.
- Mattey DL, Thomson W, Ollier WE, et al. Association of DRB1 shared epitope genotypes with early mortality in rheumatoid arthritis: Results of eighteen years of followup from the Early Rheumatoid Arthritis Study. Arthritis Rheum 2007;56(5):1408-1416.
- Gonzalez RP, Falimirski M, Holevar MR, et al: Surgical management of renal trauma: is vascular control necessary?, J Trauma 47(6):1039n1042, discussion 1042n1034, 1999.
- Poliak S.The Main Efferent Fiber Systems of the Cerebral Cortex in Primates. Berkeley, CA: University of California Press, pp. 81-104, 1932.
- Cuscheiri A. Single-incision laparoscopic surgery. J Minim Access Surg 2011;7(1):3-5.
|